“I honestly hadn’t expected it to work.” That’s Yiyin Erin Chen, assistant professor of biology at MIT. Chen and some colleagues at Stanford had eliminated an aggressive form of skin cancer from mice — simply by rubbing a swab of bacteria on their furry little heads.
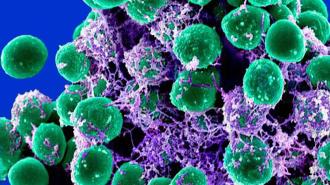
The swab contained genetically engineered forms of a bacteria called Staphylococcus epidermidis. Commonly found on human skin, Staphylococcus epidermidis is an innocuous enough passenger, minding its own business without triggering an immune response.
But when it was engineered to carry a tumor antigen, S. epidermidis was sparked an aggressive immune reaction — strong enough to wipe out skin cancer tumors in mice. The modified bacteria marshaled special immune cells called T cells to come in for the kill, functioning, essentially, like a melanoma vaccine.
“Every other type of tumor vaccine research involves radiation, chemotherapy or surgery, but we barely did anything to these mice,” Chen said.
“The T cells did the work for us.”
Researchers eliminated an aggressive form of skin cancer from mice — simply by rubbing a swab of bacteria on their furry little heads.
A spot of T (cells): Chen and Stanford associate professor of bioengineering Michael Fischbach hadn’t set out to fight skin cancer. Instead, the researchers were investigating a different immunity mystery: why do our bodies spend the time and energy to create T cells to fight the friendly Staphylococcus epidermidis?
T cells are like the immune system’s special forces. Trained to attack specific signatures on invaders — called antigens — the T cells launch from their bone marrow base and are off to attack their targets.
Weirdly, S. epidermidis causes the body to create especially potent CD8 T cells. Likened by researchers to the immune system’s “main battle tank,” CD8 T cells come bearing a plethora of molecular weapons that allow them to attack and destroy cells displaying their antigen target.
But the CD8 T cells produced by the presence of S. epidermidis don’t seem to do anything at all. It’s like a whole armored division just sitting around idling.
T cells vs. tumors: The team figured out a way to put the fleet of lazy, S. epidermidis-targeting T cells to work — the tanks just needed a new target.
In their study, published in Science, the team engineered S. epidermidis to produce a different type of antigen. Called ovalbumin, the antigen has been incorporated into many mouse tumor lines, including an aggressive melanoma.
The team then swabbed mice with either the live engineered S. epidermidis, a version that had been killed, the friendly wild-type bacteria, or no bacteria at all. Six days later, the mice were injected with melanoma cells that expressed ovalbumin.
By engineering a friendly bacteria to produce a tumor target, the immune system’s T cells could be trained to fight cancer.
Mice who had gotten the wild-type or killed bacteria — or no bacteria at all — rapidly developed skin tumors. The mice who got the live engineered S. epidermidis saw slowed tumor growth, or no growth at all. The CD8 T cells sparked by the bacteria had spread throughout the body, now hunting down their cancerous foes.
“Watching those tumors disappear — especially at a site distant from where we applied the bacteria — was shocking,” Fischbach said. “It took us a while to believe it was happening.”
To determine if their engineered bacteria could work as a treatment for already-developed cancer, the team then injected cancer cells into mice two weeks before swabbing them with the engineered bacteria.
Even when the cancer had made it to the lungs, the CD8 T cells sparked by the Staphylococcus epidermidis were able to shrink or eliminate tumors, improving the survival time of the mice. When the bacteria were combined with a type of immunotherapy that’s meant to hypercharge T cell activity, it was even more effective, clearing 15 out of 16 established tumors and preventing tumor growth when the mice were re-injected with cancer cells 30 days later.
“This appears to be evidence of a memory immune response similar to what happens after a vaccine,” Fischbach said.
“Watching those tumors disappear — especially at a site distant from where we applied the bacteria — was shocking. It took us a while to believe it was happening.”
Michael Fischbach
Not here yet: Of course, there’s a major caveat here: the new treatment has thus far only been tested in mice. However, the researchers do have some reason to be hopeful; previous studies have shown that S. epidermidis causes the creation of CD8 T cells in primates as well as mice, and humans are its favorite home.
“Human skin is the natural home for staph epidermidis,” Fischbach said. “In humans, the bug will colonize more efficiently, potentially leading to a constantly renewing supply of tumor-specific T cells.”
If the therapy proves to work, the researchers envision using engineered colonizing bacteria to harness an immune response against any number of cancers and diseases.
“If we can direct even a bit of this immune attention toward specific cancers — or potentially infectious diseases — we will have a very effective, low-cost therapy that can simply be applied to the skin,” Fischbach said.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].