A relatively new way to attack cancer, called immunotherapy, is revolutionizing cancer treatment by enabling patients’ own immune systems to attack cancer cells. It hasn’t worked for many kinds of cancers, though — evading the immune system is one of the first tricks that cancer learns. As it turns out, many cancers are also pretty good at hiding from immunotherapies.
In a recent study published in the journal Science, though, Salk Institute researchers have discovered a new way to make cancer visible to immunotherapy. To do this, the team reprogrammed mitochondria — the organelle widely memed as the “powerhouse of the cell” — to make cancer cells easier to find and kill.
The engine of cancer: What connects mitochondria and cancers? Another hallmark of cancer is their uncontrolled growth. Fueling this rapid and relentless proliferation requires a lot of energy. This increased demand is met by changes in how mitochondria function in cancer cells.
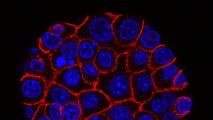
The way that mitochondria create energy for the cell is highly sophisticated, but you can imagine it working kind of like a hydroelectric dam. The mitochondria’s membrane is like a dam, dotted with protein complexes that work like “floodgates,” controlling the flow of electrons and protons across the membrane.
Mitochondria’s involvement in cancer growth goes beyond a simple increase in energy production.
These gates create an imbalance between levels of protons on either side of the membrane. Similar to how moving water powers a turbine, a flow of protons can then move an enzyme that facilitates the synthesis of ATP, the energy currency of the cell.
Researchers are also learning that mitochondria’s involvement in cancer growth goes beyond a simple increase in energy production. The transition from healthy to cancerous cells involves a complete overhaul of cellular metabolism, and mitochondria play a key role.
In fact, studies show that many cancers can actually steal mitochondria from T cells, the immune cells that typically identify and destroy threats to the body. This is a double whammy that strengthens cancer cells while weakening immune cells. This may be one of the key ways cancer thwarts immunotherapy — T cells move in to attack and get weakened by the cancer they’re trying to target.
In many studies, the state of mitochondria in tumors has been determined to be an indicator of patient response to immunotherapy. This raises the question: can we change the mitochondria in cancer cells to make them visible to immunotherapy?
This marked previously hidden tumors as targets for immune cells.
Hacking mitochondria: The team genetically engineered mouse melanoma cells to delete the genes for certain membrane complexes (either “complex-I,” CI, or “complex-II,” CII). Knocking out either complex meant that electrons were forced to flow through the other complex. In both cases, other complexes functioned as usual but the rate of respiration (or energy production) dropped. Tumor proliferation, which requires considerably higher energy, therefore also slowed down.
Another key finding showed how mitochondrial activity directly interacts with the immune system.
One of the ways that cancer cells escape the immune system is by losing proteins on their surface that immune cells bind to (called the “major histocompatibility complex,” or MHC). In their experiment, knocking out CII in the mitochondria led to the overproduction of succinate, a metabolite known to initiate tumor formation. However, this also triggered the expression of immune genes, subsequently generating MHC proteins on the surface of tumor cells. In other words, this marked previously hidden tumors as targets for immune cells.
“These findings change how we now think about future treatment strategies.”
Karthik Varanasi
The team further demonstrated this by knocking out a gene that rewired mitochondria to make electrons flow preferentially through CI, also achieving the immune-boosting effect without disrupting ATP production or other obvious adverse effects.
“We think we found a novel mechanism by which antigen presentation in tumor cells is regulated,” said co-first author Karthik Varanasi. “These findings change how we now think about future treatment strategies.”
What’s next? Multiple clinical trials are already underway to repurpose drugs that target different parts of the mitochondrial metabolism for cancer treatment. This study illustrates that richer insights on mitochondrial metabolism could also improve success of cancer immunotherapy.
While this study shows one pathway to make cancer immunotherapy more potent, details of the underlying mechanism are still missing, and turning this discovery into a treatment will take a lot of work. Moreover, in clinical use, shutting down CII activity broadly could have adverse effects, including damage to the nervous system.
Researchers are now investigating methods to deliver succinate directly to cancer cells, which might achieve the same anticancer effect without the complexity or side effects of interfering with mitochondria at all.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].