Since retiring from Microsoft, Bill Gates has spent a lot of time thinking about how to save humanity — and from what, exactly, we most need saving.
There is no shortage of candidates, but squarely at the top of his enemies list sits a deceptively small foe, which he calls the deadliest animal in the world: the humble mosquito.
Carrying plagues such as malaria, dengue, yellow fever, Zika, and West Nile, mosquitoes are responsible for half a million deaths every year (overwhelmingly, children in sub-Saharan Africa), while further racking up hundreds of millions of nonfatal infections.
Besides much other suffering, mosquito-borne illnesses contribute to countless miscarriages, premature births, birth defects, and developmental issues for children in malarial regions.
The most ambitious plan to save the world from this menace is simple: create a safe, reliable, publicly accepted, and ecologically sustainable way to wipe out mosquitoes that can carry disease.
Using the latest genetic technology, Target Malaria (supported by the Gates Foundation, other charities, governments, and aid groups) is teaming up with scientists across the developing world to extinguish mosquito populations.
In an era when heroic efforts are being launched to save species from extinction, it’s a stark contrast to see some of our brightest and most public-spirited minds striving to push a couple more into the evolutionary dustbin.
But before scientists unleash on the mosquito, they want to the public to be firmly on their side, and that means answering a lot of questions about the technology and convincing a skeptical public that their plan is safe, sensible, and necessary.
Why Pick on Mosquitoes?
There are thousands of diseases out there, and there’s no objective way to rank them. Many of the largest killers in terms of sheer numbers (cancer, heart disease, and stroke) primarily affect older people, and you might choose to put more weight on diseases that hit children hardest, cutting short lives that have scarcely begun.
We also might want to consider quality of life, not just quantity, because some diseases are debilitating, recurring, or cause more suffering than death tolls alone can capture.
There’s also a cost/benefit question: where can we do the most good? A dollar donated to one cause just might not do as much good as a dollar somewhere else. Even if we settled on what the “worst” disease is, maybe we could save more lives by targeting the second worst.
These questions are difficult and perhaps impossible to answer. But if you made a kind of Venn diagram of these factors — death toll, age of victims, severity of illness, non-fatal cases, and cost effectiveness of prevention/treatment — somewhere smack in the middle would be malaria and other mosquito-borne diseases.
In 2017, the death toll from malaria was as low as 401,000 and perhaps as high as 840,000 people (depending on whose data you trust). All sources, however, continue to show that young people are by far the hardest hit, with children under five accounting for 60-70% of all deaths.
The Against Malaria Foundation tries to contextualize those huge numbers with an analogy:
Every day, more than 500 people die from malaria in the Democratic Republic of Congo, and the majority of these deaths are children under the age of five. … Imagine a fully booked 747 airplane and infants strapped into seats A through K of every row of the economy section; their feet cannot reach the floor. Every day, this plane disappears into the Congo River, killing every soul on board. That is malaria — in one country.
Surprisingly, malaria actually isn’t all that deadly — only a small fraction of those who contract the parasite will die from it. But because over 200 million people are infected every year, according to WHO estimates, even a low mortality rate can lead to hundreds of thousands of deaths.
Over 90% of both malaria cases and fatalities occur in sub-Saharan Africa, and the numbers suggest that something like 1 in 5 people in sub-Saharan Africa deal with malaria each year (although the percentages vary widely between countries). The burden of the disease on both the health and economic development of poor countries is heavy and persistent.
Mosquitoes also transmit other nasty diseases, like yellow fever and dengue, that likely kill a further 50-80,000 people, and even fairly minor infections like Zika can lead to major birth defects if contracted during pregnancy.
This is to say nothing of the trillions of infuriating, itchy, and painful bites that mosquitoes inflict, or all the costly efforts to control mosquito populations.
Why Haven’t We Fixed It Already?
Fighting malaria is routinely cited as one of the most cost-effective ways to save a life, and, in response to worldwide efforts to distribute insecticide and bed nets, deaths from the disease fell sharply beginning in the early 2000s.
Unfortunately, progress has stalled in recent years, and the total number of malaria cases has even begun increasing again since 2015. Funding for malaria control has flatlined, and many ambitious vaccine projects have flopped when tried in the real world.
This isn’t the first time that progress against the disease has stalled after a string of major successes.
Until 1951, malaria was endemic throughout the southern United States, when a four-year blitz combining the powerful insecticide DDT, swamp drainage, and other efforts managed to eradicate malaria-carrying mosquitoes.
Europe, Russia, China, and many other temperate regions were also able to extinguish the disease using these methods. Yet the global campaign to eradicate malaria petered out soon afterward. Public health authorities simply failed to appreciate how much more difficult eradication would be in poor, tropical, and unstable regions that had vastly stronger mosquito populations.
The CDC’s postmortem on the effort attributes the failure to many factors:
Some nations were excluded completely from the eradication campaign (most of sub-Saharan Africa). The emergence of drug resistance, widespread resistance to available insecticides, wars and massive population movements, difficulties in obtaining sustained funding from donor countries, and lack of community participation made the long-term maintenance of the effort untenable.
DDT was eventually banned or heavily restricted throughout the world in the 1970s because of environmental concerns, but by then, overuse had bred resistance to the chemical into many mosquito populations.
In recent years, health officials have settled for a more modest goal of “controlling” malaria, rather than eliminating it. Distributing bed nets and spraying indoors to repel (rather than exterminate) mosquitoes was seen as the best we can do.
Now, that strategy is also stalling, with funding stagnant and malaria on the rise in Africa again. Fighting malaria may still be the cheapest way to save a life, and vast progress has been made, but it just isn’t as easy as it used to be.
The Science of Extinction
Now, a pair of new technologies has burst onto the scene, presenting a completely new way to attack the problem.
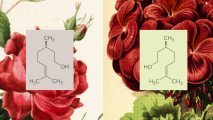
First, the revolutionary gene-editing tool known as CRISPR-Cas9 has allowed scientists to cut and paste genes with pinpoint precision, allowing us to make specific, deliberate changes to a species’ DNA. Second, using a technique known as a “gene drive,” scientists can make sure that a genetic change is passed down to 100% of an animal’s offspring.
Combined, these methods offer us our first real shot at defeating mosquito-borne illnesses, rather than simply managing them.
First, scientists used CRISPR to insert a gene that makes female mosquitoes (the ones that actually bite humans) infertile. When they have a copy of this gene, females won’t be able to bite people or reproduce — but the nonbiting males can reproduce, mating with unaltered females and spreading the infertility gene.
It sounds like the story should end here — just snap the gene into some males and let them go. But there’s a problem: like humans, mosquitoes have two copies of every gene (one from each parent). When they make sperm or eggs, they randomly discard half their genes, so only half of their offspring will end up with any given gene.
A gene for female infertility means that not only will daughters not pass it on, only half of their sons will get it, too. And those males will only give it to half of their sons, and so on. Natural selection will punish mosquitoes with this gene, compared to those who have fertile daughters, and it’ll get whittled down out of the population pretty quickly.
A “gene drive” is a way of hacking this system to make sure that 100% of their offspring will inherit a particular gene. Gene drives exist in nature, but they’re rare and random. Now, scientists have figured out how to design them on purpose.
By attaching the CRISPR tool itself to the gene for infertility, scientists can order the gene to copy itself to the other half of the mosquito’s genome. In other words, they’ll now have two copies instead of just one, so all of their offspring will inherit it.
Using this technique, males can quickly spread a gene for female infertility throughout the mosquito population, until eventually there are not enough fertile females to carry on the population.
This method has been successfully tested in the lab, with caged mosquito populations completely dying out in just six months.
The gene drive looks like the ultimate weapon on stop the spreading of mosquito-borne disease.
So… Is There Any Reason Not to Do It?
In some ways, gene drives are highly targeted. They will stay in their lane and only hit the species they’re designed for — for instance, Anopheles gambiae, one of the primary carriers of malaria, or Aedes aegypti, which carries yellow fever and Zika virus.
But in other ways, they’re harder to control. Once released into the wild, they are designed to spread throughout the entire population. That means they won’t respect national boundaries and won’t stay in a particular place.
Scientists are developing techniques to limit gene drives, but, either way, Target Malaria and other groups will need to get buy-in from everywhere that could be affected by releasing the gene drives into the wild.
There are also obvious environmental concerns about disrupting ecosystems. Some environmental groups are already calling for a preemptive moratorium on gene drives, arguing that we shouldn’t tamper with the natural order. In some places, mosquitoes play a big role in wildlife food chains, so we wouldn’t want to wipe them all out even if we could (and we almost certainly can’t).
The good news is that only about 200 of the 3,000 mosquito species even bite humans, and only a handful are responsible for the really dangerous diseases like malaria and dengue. For better or worse, the ecological niche of buzzing, bloodsucking parasite is in no danger of being emptied.
Ultimately, extinction of even one species probably isn’t a practical goal (although we can always dream). First, the world is simply vast. It’s far more likely that the gene drives would burn themselves out — dying off with a local population before it could get all the way across a rainforest or continent — than it is that it would sterilize the whole species.
Second, there’s a reason why gene drives are rare in nature: species are under the strongest possible evolutionary pressure to develop resistance to them. Scientists are well aware of the problem of resistance, and they’re taking steps to prevent it — but as the biologist Leslie Orgel once quipped, “Evolution is cleverer than you are.”
Evolution and genetics are complicated, and it’s not always clear whether stuff that works inside the lab will succeed outside it, or for how long.
What Next?
Target Malaria, researchers at Imperial College London, and other pro-gene drive groups are proceeding with immense caution. They have tested the drives in the lab, but they are planning a slow, long testing campaign in labs in malarial areas, experimenting on caged local mosquito populations to test it under realistic circumstances.
Their goal is to be embedded in local communities and demystify the concept of genetic engineering, showing people what they’re doing (and why) and earning public trust through transparency.
In the meantime, the scientists are continuing to look for a remote island somewhere that would give them permission to test a gene drive in the wild, without worrying that it could spread elsewhere.
The commitment to getting public support is admirable, but now changes the nature of the problem from a technical challenge to a social one.
UC-San Diego’s Ethan Bier is working on a gene drive that spreads a gene that makes mosquitoes resistant to malaria, rather than making them infertile. When Vox’s Dylan Matthews asked him “how soon a drive targeting malaria could be released, as a scientific matter”:
Bier hesitated, and stressed that we shouldn’t release anything without regulatory approval and much more consideration. But he concluded, “To be honest with you, if there were some kind of emergency and one absolutely needed to do it, we could pretty much do it.”
Bier and some others suspect that the public could be more accepting of a genetic change that would stop mosquitoes carrying malaria, rather killing them off outright. But either way, they’re very clear that they won’t make a move without widespread local support.
Particularly in a region like sub-Saharan Africa, that means reaching out and gaining the trust of not just the public but also many national governments (by no means all democracies), hundreds of tribal, religious, or ethnic groups, and countless villages in rural areas.
There’s a lot of public mistrust of health authorities throughout Africa — not always without reason — and there’s a history of heavy-handed and counterproductive interventions by well-meaning foreign experts. It’s a difficult collective action problem, so they’re taking it slow, mainly hoping to forestall a ban on the technology until they can build up support and evidence for its safety and efficacy.
Ultimately, the dream of wiping out all mosquitoes that prey on humans is probably unattainable. But wiping out mosquito-borne diseases like malaria is still very much achievable, and genetic technology (along with anti-malarial drugs, bed nets, insecticides, and perhaps someday also vaccines) could be our best shot at it in a very long time.