One genetic mutation appears to dramatically increase a person’s chances of feeling fine during a COVID-19 infection, according to a new study — and the discovery could lead to new drugs and vaccines that help even non-mutants avoid getting sick.
Asymptomatic COVID: Most people who catch COVID-19 will have mild to moderate symptoms — a miserable few days or weeks — and a smaller number will develop severe cases, ending up in the hospital or worse. But research suggests that at least 20% (and potentially more) of those infected with the virus are asymptomatic.
These “silent infections” play a big role in spreading the virus, but they are also important because if we can figure out why some people don’t get sick, we might be able to help those who do.
At least 20% (and potentially more) of those infected with the virus are asymptomatic.
In search of an explanation, a team led by Jill Hollenbach, an immunologist at UC San Francisco, turned to the National Marrow Donor Program (NMDP), which collects DNA samples from people willing to donate bone marrow for transplants.
Through an email campaign, launched in July 2020, the researchers found nearly 30,000 people willing to use an app to complete a survey and answer daily questions about any symptoms they were experiencing and weekly questions about COVID-19 testing.
Within that group, 1,428 unvaccinated participants reported testing positive for COVID-19 between February 2020 and April 2021. Of those, 136 people said they experienced no symptoms for two weeks before and two weeks after testing positive.
“It was a really clear, robust, and replicable association.”
Jill Hollenbach
In their genes: When the researchers looked at the DNA samples of people who tested positive for COVID-19, they discovered that 20% of those who were asymptomatic had a specific genetic mutation — HLA-B*15:01 — compared to only 9% of those who experienced symptoms.
Meanwhile, people who had two copies of the mutation — one from each parent — were eight times more likely to experience asymptomatic COVID than people with no copies.
“To be fair, not everybody that has [HLA-B*15:01] will be asymptomatic,” Hollenbach told NPR. “But it was a really clear, robust, and replicable association.”
How it works: Typically, the immune systems’ T cells only react to the COVID-19 coronavirus if they’ve seen something just like it before — either by priming with vaccination or a prior infection.
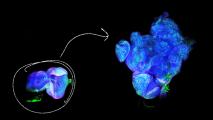
Based on lab tests, the researchers believe that this mutation allows T cells to be primed by other coronaviruses — such as the ones that cause the common cold — to also immediately recognize the COVID-19 virus as a threat.
“If you have an army that’s able to recognize the enemy early, that’s a huge advantage.”
Jill Hollenbach
Their theory is that this cross-immunity allows the T cells to launch a swift defense against COVID-19, preventing the development of symptoms.
“If you have an army that’s able to recognize the enemy early, that’s a huge advantage,” said Hollenbach. “It’s like having soldiers that are prepared for battle and already know what to look for, and that these are the bad guys.”
The cold water: The researchers’ primary study group (those analyzed after testing positive for COVID-19) was not diverse, with 100% self-identifying as white and 81% as female, so more research is needed to confirm the results in other groups.
“In terms of diversity, we cannot expand these results to all populations because we know, based on epidemiological reports, COVID symptoms vary across populations,” Samira Asgari, an immunologist at Mount Sinai, who was not involved in the study, told the Washington Post.
“This might enable us to identify new ways of promoting immune protection.”
Stephanie Gras
Looking ahead: Now that HLA-B*15:01 has been identified as playing a role in asymptomatic COVID, the next step is pulling on that thread with future studies, including ones in which researchers take a closer look at the immune systems of people with the mutation.
“By studying their immune response, this might enable us to identify new ways of promoting immune protection against SARS-CoV-2 that could be used in future development of vaccines or drugs,” said researcher Stephanie Gras from La Trobe University.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].