It sounds innately bad, but the presence of viable bacteria in the blood — called bacteremia — isn’t always an emergency. It can occur after brushing a bit too vigorously, say, or from a medical procedure.
But if the immune system fails to keep them in check, bacteremia can become a bloodstream infection (BSI), a potentially lethal condition with mortality rates potentially pushing 40%, depending on patient and pathogen.
According to researchers at the University of Toronto, two million cases of bloodstream infection happen in Europe and North America annually. Those cases are associated with 250,000 deaths, making bloodstream infection the leading cause of death by infection.
A bloodstream infection is a potentially lethal condition, with mortality rates pushing 40% if not caught early.
When minutes count: Detecting a bloodstream infection early, and administering the proper treatment, significantly improves patient outcomes, but there’s a catch: rapid diagnosis is difficult.
The current gold standard, which involves growing a blood culture and using PCR testing, can take days, when some patients may only have hours.
Now, University of Illinois bioengineering professor Rashid Bashir and his lab have developed a new test to identify blood-borne pathogens much faster, using a two-step blood drying process.
“Alternatively, our approach using a new blood drying technique can be used to detect pathogens in less than a few hours,” Bashir told Inside Precision Medicine (IPM). “This can potentially be very important for rapid and early detection of onset of sepsis caused by bacteremia.”
To the test: The Bashir team’s method, published in PNAS, allows pathogen DNA to be amplified to detectable levels from 1 ml of whole blood — producing bloodstream infection results within 2.5 hours, IPM reported.
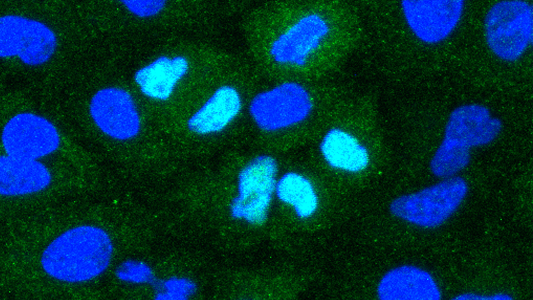
To do this, they use a novel, two-step blood drying process to alter the blood’s structure and deactivate the various blood components — like platelets, cells, and proteins — that can interfere with testing.
The blood is first rapidly dried at temperatures up to 203 F, IPM explained, which deactivates these components and stops the blood from taking part in the chemical reactions driving the test.
By hitting the blood sample with heat again, the team caused it to become more porous, allowing the enzymes to better access whatever pathogenic DNA may be in there, ending with faster results.
The new test can deliver results within hours, not days, which would allow treatment to be provided quicker.
The researchers were able to detect a variety of pathogens, including the bacteria Staph. (MRSA and regular), E. coli, and even a fungal pathogen, Candida albicans.
When compared to 63 samples that used the culture and PCR method, the new test showed perfect agreement — 100% sensitivity and specificity, meaning it caught all of the true positives and identified all of the true negatives.
The future: With rapid diagnosis, patients could receive treatment much earlier in the course of their bloodstream infection — and be more likely to survive it. And by using fewer instruments and less complex procedures, the test could be especially impactful in the developing world and locations with limited resources, the authors wrote.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].