Doctors may be able to improve outcomes for patients with head and throat cancers simply by injecting the common local anesthetic lidocaine near the site of their tumors, according to a new University of Pennsylvania study.
The background: Cells on the surface of your taste buds express proteins called “bitter taste receptors” (T2Rs). When you eat something bitter, it activates these proteins, causing them to trigger nerves that send signals to your brain that give you the sensation of taste.
Your mouth isn’t the only place where you’ll find T2Rs, though. The cells of your heart, lungs, brain, and other tissues also produce the proteins (for reasons that aren’t entirely clear), as do a variety of cancer cells.
“We know lidocaine is safe, we’re comfortable using it, and it’s readily available.”
Ryan Carey
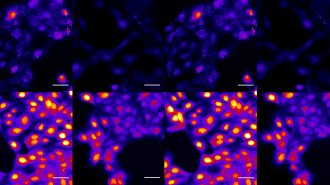
What’s new? In 2022, Penn scientists discovered that many head and neck cancers contain T2Rs and that activating the proteins with bitter compounds triggers cellular death. They also identified an association between increased T2R expression and better patient outcomes.
In a new study, they reveal that lidocaine can activate T2R14 — a bitter taste receptor found in high levels in many cancer cells — leading to cell death.
“Speaking as a head and neck surgeon, we use lidocaine all the time,” said co-lead researcher Ryan Carey. “We know lidocaine is safe, we’re comfortable using it, and it’s readily available, which means it could be incorporated into other aspects of head and neck cancer care fairly seamlessly.”
The big picture: Lidocaine was already suspected of being beneficial to cancer patients prior to this study, but researchers didn’t know why or how it seemed to help.
The Penn study not only reveals that the drug activates T2R14 to trigger cell death, but also identifies two mechanisms that enable this activation: mitochondrial calcium ion overload and proteasome inhibition.
“While we’re not suggesting the lidocaine could cure cancer … it could get an edge on head and neck cancer treatment.”
Ryan Carey
This improved understanding of the process could lead to new cancer treatments and paves the way to clinical trials in which the anesthetic is administered alongside standard cancer therapies.
“While we’re not suggesting the lidocaine could cure cancer, we’re galvanized by the possibility that it could get an edge on head and neck cancer treatment and move the dial forward, in terms of improving treatment options for patients with this challenging form of cancer,” said Carey.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].