In a first-of-its-kind trial, Johns Hopkins University researchers deliberately exposed 20 women to the Zika virus — and the fact that they were all infected is actually really great news for vaccine developers.
The challenge: In the final stage of vaccine development, researchers will usually enroll thousands of people in a clinical trial, vaccinate about half, and then send them all back out into the world. Based on how many people in each group get sick, they’ll know how effective their vaccine is at preventing infections.
The rarity of Zika means vaccine developers can’t get the trial data they need for approval the usual way.
This approach works great if infections are common among a population — in 2020, it took just a few months for the developers of our mRNA COVID-19 vaccines to see enough infections in their vaccinated and control groups to know the shots were highly effective.
If an infectious disease isn’t common, though, there won’t be enough cases in the two groups to determine the efficacy of an in-development vaccine, and without proof that a shot works, developers won’t be able to get it approved.
The background: This was the situation Zika vaccine developers faced in 2017.
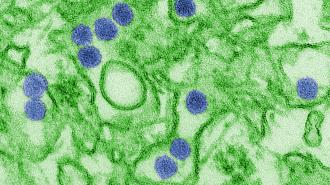
In adults, the Zika virus — spread mainly by mosquitoes — often causes mild or no symptoms (although in rare instances, it can lead to the autoimmune disorder Guillain-Barré syndrome). If a pregnant woman is infected, however, her baby can be born with severe birth defects, including microcephaly.
In 2016, the World Health Organization declared a growing outbreak of Zika a “public health emergency of international concern” and urged researchers to develop vaccines for the virus, specifically ones that could be given to pregnant women.
By 2017, though, the number of cases had plummeted, meaning those who had heeded the WHO’s call and started developing Zika vaccines were unlikely to ever get the trial data they needed to get the shots approved.
The idea: Even though Zika infections are now rare, it’s still a serious epidemic threat, and developing a proven vaccine before the next outbreak is still a major public health priority. Human challenge trials could help us develop the shots, even without much Zika out there.
In these trials, researchers deliberately expose participants to a virus, rather than waiting for them to (maybe) encounter it in the wild. This can significantly speed up vaccine development, especially in cases where natural infections are currently rare, like Zika.
What’s new? On October 21, Johns Hopkins University researchers shared the results of the first human challenge study involving the Zika virus with Nature. Then they presented their data at the annual meeting of the American Society of Tropical Medicine and Hygiene.
After splitting 20 unvaccinated women into two groups, the researchers exposed each group to a different strain of Zika. An additional eight women were given a placebo.
“You could get an efficacy result with many fewer people.”
Anna Durbin
As expected, no one in the placebo group developed a Zika infection. All of the women challenged with the virus became infected, but their symptoms were mild and temporary: 95% of them (or all but one) developed a rash and 65% experienced joint pain.
The women agreed to stay at a research facility until they were no longer infectious (9 to 16 days), and each of the 28 participants received about $5,000 for taking part in the study.
The impact: Study co-author Anna Durbin told Nature that the results of the trial suggest that either strain of Zika could be safely used in a future human challenge trial of a Zika vaccine. That trial wouldn’t need to be particularly large, either.
“With the challenge model, where you have 100% of infections, you could get an efficacy result with many fewer people,” she said, adding that 50 to 100 participants could be enough.
Even if those challenge trials suggest that a Zika vaccine is effective, though, developers would still need to trial it in a few thousand people to ensure the vaccine itself is safe.
Looking ahead: The JHU team is now looking for men to participate in a second Zika challenge study. This one will also test how long the Zika virus remains infectious in semen, which could potentially help prevent sexual transmission of it in the future.
Durbin told Reuters several vaccine manufacturers have already reached out to ask about using the Zika strains from the challenge trials to “test experimental products.”
None of the teams developing Zika vaccines have announced plans for human challenge trials, but ultimately, they might be the only way to prove the shots’ efficacy and ensure we don’t have to battle another Zika epidemic in the future.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].