This article is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.
Your immune system is like a security guard for your health. Day and night, it’s patrolling your body, looking for any suspicious characters — viruses, cancer cells, etc. — so that it can attack and eliminate threats that can make you sick.
If you have an autoimmune disease, though, your immune system mistakenly attacks your own healthy cells, tissues, or organs.
“The effects of autoimmune disease are devastating,” Olivia Casey, senior director of programs at the Autoimmune Association, and Frederick W. Miller, a National Institutes of Health Scientist Emeritus, wrote in Scientific American. “As a person’s own immune system attacks their body instead of microbes or cancerous cells, they can experience chronic fatigue, chronic pain, drug dependency, depression, and social isolation.”
An estimated 24 million Americans have at least one autoimmune disease.
There are more than 80 known autoimmune diseases, and the most common treatment for many of them — if one exists at all — are drugs that suppress the activity of the immune system, but they come with a trade-off: a weakened immune system that leaves a person at increased risk of infection.
This isn’t a rare problem, either. An estimated 24 million Americans have at least one autoimmune disease (unluckily, people who have one condition are at higher risk of developing more), and these conditions appear to be getting more prevalent, too.
This makes figuring out a better way to treat all of these people — or maybe even cure their diseases — more important than ever, and researchers are currently pursuing several promising leads.
Inverse vaccines: Teaching tolerance
The idea: Vaccines introduce “antigens” — the part of a pathogen that triggers an immune response — to your immune system so that if you are ever infected in the future, your immune system will recognize the antigen and attack it right away.
To cure autoimmune diseases, researchers at the University of Chicago want to do the opposite, by developing inverse vaccines to get the immune system to tolerate harmless things.
How they work: When the liver filters your blood, it “tags” your body’s old, broken down cells so that they can die of natural causes without riling up the immune system. (This phenomenon is called “peripheral immune tolerance.”)
There may be a way to use this tagging system to tell the immune system to leave things alone. By adding a sugar molecule called pGal to cells they wanted the immune system to tolerate, the Chicago researchers found they could get the liver to stick an “ignore” tag on them, too.
The approach has already worked in mouse models of two autoimmune diseases — Celiac disease and multiple sclerosis (MS) — getting the animals’ immune systems to tolerate their triggers: gluten and myelin, respectively.
“We’re incredibly excited.”
Jeffrey Hubbell
The drawbacks: Lots of treatments that work in mice don’t translate to people, too, so we won’t know for sure how effective these inverse vaccines are until they prove themselves in large clinical trials.
If it works, this approach could potentially be applied to other autoimmune diseases, too, but only if we know exactly what triggers the unwanted immune reaction, and that’s not always the case.
Looking ahead: The inverse vaccine for Celiac disease has already proven safe and tolerable in a phase 1 trial, and a phase 2 efficacy trial is ongoing. A phase 1 trial for the MS inverse vaccine was underway as of September 2023.
“There are no clinically approved inverse vaccines yet, but we’re incredibly excited about moving this technology forward,” said researcher Jeffrey Hubbell.
Navacims: On the defensive
The idea: Rather than using drugs to suppress the entire immune system — and thus leaving a person at increased risk of infection — immunologist Pere Santamaria from the University of Calgary is developing a therapy, called Navacims, that targets only troublesome immune cells.
How it works: Navacims are nanoparticles that Santamaria’s team has covered in proteins that act as “bait” for the white blood cells that are causing an autoimmune disease. Once they catch their target, they reprogram it from a “killer” cell into a “regulatory” cell — the purpose of those cells is to keep your immune system from overreacting.
“Those [reprogrammed] white blood cells can only disband inflammation in the organ that they were attacking in the first place, so basically converting an attack into a defense,” said Santamaria.
“[It] requires a lot of time and resilience with a lot of rejection and failures along the way.”
Pere Santamaria
The drawbacks: Navacims have shown promise in lab tests and mouse models against a handful of autoimmune diseases, including type 1 diabetes, inflammatory bowel diseases, and MS — but there’s still a lot of work ahead.
“It’s not straightforward to bring pharmaceutical products from the bench to bedside,” Santamarie told Avenue Calgary in 2021. “To take a discovery from the research laboratory to the level of building a new class of drugs, and then to clinical trials, requires a lot of time and resilience with a lot of rejection and failures along the way.”
Looking ahead: Navacims might be unproven in people, but that hasn’t stopped Parvus Therapeutics — a startup co-founded by Santamaria and the University of Calgary — from securing more than $1 billion in licensing and partnership agreements for the nanoparticles.
The startup will reportedly launch its first clinical trial in 2024, with Navacims targeting an autoimmune liver disease.
CAR T-cells: From cancer to lupus
The idea: During CAR-T cell therapy, T cells — a type of immune cell — are removed from a cancer patient’s blood and engineered to display proteins that will bind to their cancer cells. When the T cells are put back into the patient’s body, they direct the immune system to attack the cancer.
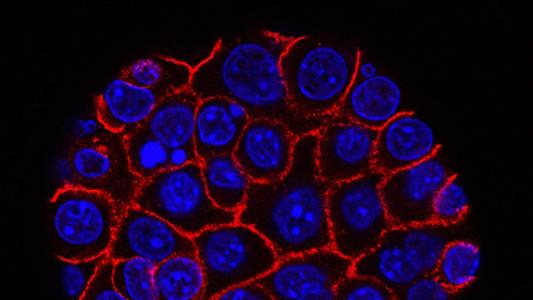
Researchers in Germany are working to convert this powerful cancer treatment into a cure for lupus, an autoimmune disease in which the immune system’s B cells create autoantibodies that attack the body’s own cells.
How it works: The German team engineered its T cells to display proteins that bind to (or target) the abnormal B cells that are causing lupus, essentially pitting the immune system against itself.
Eight patients with treatment-resistant lupus who underwent the therapy experienced a depletion in abnormal B cells, and when their bodies started making new B cells, they didn’t create the autoantibodies.
“All lupus patients, as of today, don’t show any symptoms, and they are completely free of treatment,” study leader Fabian Mueller told attendees at the American Society of Hematology’s annual meeting in December 2023. “At this time, with limited follow-up, we say that [the treatment] achieves a lasting remission in [the most common type of lupus].”
The treatment could be a way to manage lupus without putting patients at increased risk of infection.
The drawbacks: The treatment still needs to prove itself in larger studies, and we don’t know exactly how long remission might last — the median follow up in the 2023 study was 15 months.
CAR-T cell therapy for cancer is also incredibly expensive — a single infusion can cost nearly half a million dollars in the US — and the treatment can cause serious adverse effects, including cytokine release syndrome (CRS), which can be fatal.
Looking ahead: The CAR-T cell therapy has been well tolerated in lupus patients so far, and Schett believes the risk of CRS following this therapy is inherently lower for lupus than cancer.
“The difference between cancer and autoimmunity is that in cancer, there are usually more cells involved … Whereas in autoimmunity, the number of B cells is much lower, and therefore it seems that the safety profile of CAR-T cell therapy and autoimmunity is much better than in cancer,” Schett told Wired.
If the therapy proves itself in larger, longer trials, it could give us a way to manage lupus — and maybe other autoimmune disorders driven by abnormal B cells — without putting patients at increased risk of infection.
Best of the rest
These aren’t the only promising leads in the hunt for a cure for autoimmune diseases.
- Researchers have found connections between some autoimmune diseases, including MS, lupus, and rheumatoid arthritis, and the gut microbiome — the collection of microbes that live in the human digestive tract. This suggests that we might be able to treat, or even cure, the diseases by manipulating the composition of the microbiome.
- Autoimmune diseases tend to run in families, which suggests there’s likely a genetic cause for many of them — in 2022, for example, researchers identified a genetic mutation they believe is responsible for lupus. While gene editing in people is still very new, it’s possible we could one day use CRISPR to correct the mutations causing autoimmune diseases.
- A functional cure for type 1 diabetes — one of the most common autoimmune diseases — is already FDA approved for people whose condition is hard to manage. That treatment requires sourcing insulin-producing cells from donor pancreases, but if researchers can succeed in making them from stem cells, the supply will be virtually unlimited, and the cure could become widely available.
- The Epstein-Barr virus (EBV) infects 90% of people at some point in their lives, and while infections are often asymptomatic, they dramatically increase your risk of later developing MS. If we can prevent EBV infections, we might also be able to prevent MS, and several EBV vaccines, including one by Moderna, are now in clinical trials.
If even one of these promising treatments is approved, it could be life-changing for millions of people. If several of them pan out, we could be headed toward a future in which being diagnosed with an autoimmune disease isn’t the devastating news it is today.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].