The first great love of Judith Grisel’s life came to her in many forms: there were joints, spliffs, bowls, bongs — an entire emerald parade of ways to get high.
Addiction and the brain are star-crossed bedfellows. Marijuana offered a glimmering sheen to life: a sparkling Snapchat filter for the ordinary. On an adolescent trip to the mall, dull retail shops became bazaars full of wonder, and the food court pizza she and her friend devoured was, bar none, the finest pizza she had eaten in her life.
That same insatiable drive to use was turned to figuring out why Judith wanted to use. Could a key be found inside the brain?
In Never Enough: The Neuroscience and Experience of Addiction, Grisel likens her first drink at 13 to Eve biting into the apple. While marijuana was her first love, she had no one drug of choice: cannabis burned, alcohol flowed, cocaine ran down syringes into the blood — until eventually it became too much. A haunting encounter with her own reflection — the abyss in her eyes — and a breakdown during a family dinner set Grisel on the path to sobriety.
That same insatiable drive to use was turned to figuring out why she wanted to use. Could a key be found inside the brain? Now a behavioral neuroscientist and professor of psychology at Bucknell University, Grisel has dedicated her adult life to attempting to unlock the mysteries of addiction and the brain.
Freethink spoke with Grisel about understanding addiction, the chemicals inside our brains, how society sees addiction, and why freebasing moon rocks is the only thing that gets Krusty the Clown back to normal anymore, all with the intention of understanding addiction.
This interview has been edited for length and clarity.
Freethink: Can you give me an idea of what neurotransmitters are, their purpose, and how they impact the central nervous system?
Judith Grisel: The brain works by electrochemical signaling. It conveys information — information like how we feel and think and behave — with electricity.
But electricity won’t jump a broken wire, so between cells is a little gap, it’s like a broken wire, and it uses chemicals to transmit information — feelings, thoughts, behaviors — in brain circuits, and those chemicals are called neurotransmitters.
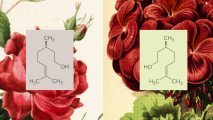
And there’s dozens, hundreds of them. All different kinds, different molecular classes, things like dopamine, serotonin, endorphins, anandamides. So lots of really interesting chemicals work between cells to convey information.
Freethink: What neurotransmitters have you found so far to be most active, in this biology of addiction?
Judith: Well, probably the core neurotransmitter is dopamine. And every single addictive drug, or even addictive behavior, is that way because it causes the release of dopamine in a particular area, called the nucleus accumbens.
Neurons get activated, in response to addictive drugs, to squirt out dopamine in the nucleus accumbens. And that gives us this pleasurable feeling of being enhanced, of really liking what we’re experiencing — a lot like you would have with sexual foreplay, or with anticipating opening a present, or having a really delicious meal, or listening to great music.
“We don’t have any notion really at all of what the balanced state is, what a normal brain looks like, in terms of all these electrical-chemical signals.”
Judith Grisel
That kind of titillating feeling of pleasure is produced by dopamine in this small part of the brain, about 2 inches behind your eyeballs, called the nucleus accumbens, and every drug that’s addictive, is addictive because it causes that activity.
Freethink: We used to have this idea for mental health disorders that the brain chemicals are sort of off, imbalanced, or something like that. And it doesn’t seem like that’s the prevailing theory anymore. It’s moved more towards this idea of a brain operating as a collection of circuits: something goes wrong in the circuits, you end up with a mental health disorder. So how do those neurotransmitters potentially impact those circuits?
Judith: First I want to say something about the old idea, which is that we thought that it would be really simple, like you just have an imbalance in dopamine or an imbalance in serotonin. What’s been enlightening on a good day (and frustrating on a bad day) is that we don’t have any notion really at all of what the balanced state is, what a normal brain looks like, in terms of all these electrical-chemical signals.
In fact, we haven’t even discovered all the neurotransmitters there are.
So we’re kind of in the dark about that. An anxiety disorder where someone won’t leave their house — or schizophrenia, where they’re seeing things and hearing things that aren’t even present — you can’t find any major circuitry or chemical-specific problems. So that’s been a dilemma, and that’s made us move more to kind of the constellation of activity (model), in multiple regions at multiple times.
I think the causes of something as complex as behavior are often multileveled. At the molecular level, at the circuit level, at the organismal level, including your biome in your gut — the bacteria that live there, we now know, are really critical for mental health and illness. Also, your circadian signals that come from how much light you get at night and how well you sleep. And probably social and cultural things as well.
Behavior is really complex because it’s a result of so many factors, not sort of a single thing or even ten things that cause it.
Freethink: I had a friend who used to drive all the time for work, and he would smoke when he drove, and it seemed to make it that much tougher for him to quit smoking. Because he had to get in the car, and every time he got in the car, he wanted to smoke. How important is that sort of linkage to developing an addiction?
Judith: Tremendously important. It’s really classical conditioning in a way. It’s what Pavlov showed.
If the car is associated with the hit from nicotine, then you get in the car, and you’re expecting that hit from nicotine.
Your brain is prepared for that in such a way that it’s going to produce craving, and kind of a withdrawal state, so that the way to fix it is to get the nicotine.
This is a huge and really relevant problem for addicts… One (reason people relapse) is these cues in the environment that predict it. And it could be your car, but it could also be the friends you use with, it could be any other drug, it could be stress, it could be a feeling state.
If you smoke every time you’re disappointed, or frustrated, or stressed, then all of those things, just like the car, induce the craving.
There’s almost no end to the associations that people make to cigarettes, because you can smoke everywhere, but it’s the same thing for other drugs. Seeing the bar, or running into a using buddy, or looking at a spoon in a bathroom. Those things completely throw people off.
Freethink: There’s a scene in The Simpsons where Krusty the Clown is talking about how he’s done so many drugs, the only thing he can do now is freebase moonrocks. And the joke is that only gets him “to normal.” How crucial is that tolerance/dependence relationship when it comes to prolonging addiction?
Judith: I think that is addiction, actually. The brain adapts to any drug that you take regularly to change the way you feel to produce the exact opposite feeling. And therefore, you’re using only to feel normal.
If you talk to someone who’s a regular opiate user, they mostly use because they don’t want to be sick. But they don’t get high. And the reason for that is, because the drug produces a high, their brain produces suffering. So the net effect is okay, but if you don’t have it, then you’re withdrawing.
And I think that’s true with every single drug. I am dependent on caffeine. I don’t wake up in the morning until I have coffee.
“The brain adapts to any drug that you take regularly to change the way you feel to produce the exact opposite feeling.”
Judith Grisel
So this is the core message. Tolerance: because as the brain produces the opposite effect, you need more and more to achieve what you’re looking for.
Dependence: because now when the drug is gone, you’re below your normal state — not awake without coffee, for instance.
And craving: because when the cues, or the stress, or another drug comes around, you are reminded and your brain produces, again, a big opposite condition.
So tolerance, withdrawal, and craving are the core hallmarks of addiction. And they’re all caused by the brain’s adapting in the exact opposite way that the drug does.
Freethink: How has your personal experience changed how you view addiction, beyond biology? There’s this desire to demonize addicts to a degree, right? Like it must be their fault, there must be something wrong with them, they’re not right. How does being a former addict yourself change how you see addiction socially?
Judith: That’s a good question. I think my initial response was actually more like you’re describing. I think I thought when I first ended up in treatment, “Wow, I’m a black sheep. I am bad news. Something is wrong.”
I think that certainly I made some poor choices, but I also have a growing appreciation — this is more my neuroscience background — for the biological constraints that helped facilitate those poor choices and my addiction.
“Why is it, I wonder, that people who live in a pretty good state, relative to most of the people in the world, want to escape it?”
Judith Grisel
Freethink: Were there people who you’ve met along the way that would change how people think of addicts?
Judith: Yeah. I think there’s a lot of comradery and a lot of loyalty, in a way. One of the things I appreciated about being homeless was that homeless people really care for each other. In my experience, I found it was a kind of more loving community, in some ways, than my family was in some ways. I think kindness shows up in places where maybe it’s needed more.
I remember one Christmas Day, I was homeless. Me and three friends somehow scraped together enough money to go to a Chinese restaurant. And it was — when I think about it now, it sounds pathetic, because we were probably not clean, and it wasn’t a nice Chinese restaurant. But we had, whatever, $5 each, and the staff I remember being happy to see us, and we were thrilled to be there. And it was nice to have a meal. And I remember thinking that this is what Christmas is about.
Freethink: I feel that for a long time the American stance to addiction was punish instead of treat. But it seems like that’s slowly starting to change. I’m curious if you feel that is the case, and if you think part of the reason might be the opioid crisis. Not to put too fine a point on it, but because white people get affected by the opioid crisis.
Judith: Mm-hmm. Well, I certainly hope it’s changing. It absolutely needs to change. And the main reason it needs to change is because it doesn’t work. The punishment is so ineffective as a motivator. It’s just, I don’t know how much psychology we need to show that. It really rarely does anything.
I do agree though that the more people we know, the more we see, “Oh, it’s not them, it’s us.” And this is also basic psychology, where we tend to blame other people for their failings but give ourselves a break. So I think as we realize, “Oh wait, this is my spouse and my child, or my neighbor it happened to,” then all of a sudden we sort of see, “Oh, there’s more nuanced things involved here.”
Freethink: If we legalized everything — we just go hog-wild, legalize all of the drugs — would addiction jump, or would the people who are using these drugs be the people who would have used them regardless?
Judith: That’s a good question. The number of people using would probably increase, because access is a big part of it. But when they did prohibition with alcohol, what happened was fewer people used, but those who used, used more.
So I think that anytime you try to restrict something, it also creates a need and a drive to use. And this is just a fundamental way of behavior, that “don’t tell me what I’m not going to do.”
It happens the same in mice. If you give them alcohol 24 hours a day, they don’t drink that much. If you only give it to them for a short time, they load up.
So for the short term, I think it would be a problem. And for the long term, it might be better.
We’ve been talking a lot about what individuals bring to the table, but a lot of the factors have to do with how we live. I think stress is such a big catalyst for wanting to escape and enhance — and maybe not only stress, but the way a lack of opportunities for interesting, stimulating experiences would make something like cocaine or marijuana more compelling.
I think it’s important to recognize that we have to do something about these structural, institutional factors that are contributing. And those are powerful.
Freethink: The science is tough. We’re struggling. There’s a lot we don’t know, but what kind of societal or institutional measures can we take (now) to help ease addiction? I’m thinking doctors working more closely with opioid dependent patients to avoid withdrawal. Or decriminalization, so people go to therapy or rehab instead of prison. What can we do socially, while we’re working on the scientific element, to help people who are addicted?
Judith: Well, I like both of your ideas.
It takes a long while to develop an addiction because the brain is adapting, but the brain will readapt back to a free independent state, but it takes time. And I think one thing we really have to do is get over this notion that we can send someone to detox for a few days and then hope for the best, because that is completely contrary to all the science.
People need long term interventions and support, and that has to be kind of widespread. I’m thinking back to your friend who is trying to quit smoking. I mean, maybe he needs a ride to work and-
Freethink: A new car.
Judith: A new car. Well, yeah. And less stress and just more general support. I really had a lot of support, and I think that all the neuroscience we know suggest that that’s going to be very impactful.
Why is it, I wonder, that people who live in a pretty good state, relative to most of the people in the world, want to escape it? Want to change it to such a degree that they’re willing to give up so much? And I think looking at the drive to be intoxicated is really important.
I think part of it is natural, but part of it is not, and certainly the self-destructive part is not natural. We’re living with a lot of anxiety disorders, a lot of depressive disorders, a lot of addictive disorders.
I mean those things are statistically normal. And why is that? It’s not in our evolutionary interest. I don’t think it’s something that we evolved to have, a lot of anxious, depressed, addicted people. I think that we have them because we have a biological vulnerability, for reasons that we’ve talked about a little bit, and the context is kind of fostering those things.
“It takes a long while to develop an addiction because the brain is adapting, but the brain will readapt back to a free independent state, but it takes time.”
Judith Grisel
So it’s a mistake to focus on the individual, not on the context, if the changes that we need to make are broad.
Freethink: So it seems like just because our scientific understanding isn’t complete, it doesn’t mean that we can’t make societal changes to help people who are addicted or to even sort of minimize addiction. Right?
Judith: Oh, David, I think that is where, yes, I really came down. I think I was hoping for this easy brain switch, or even switches, that I could find. And I think now that the low hanging fruit is actually in … it’s not easy, but I think the most impactful interventions are not going to be, at least for the near future, biological.
Freethink: There’s just too much we don’t know.
Judith: And too much we do know. We may know the things that help: social support, time, attention.