Nearly half a billion people worldwide suffer from diabetes or prediabetes. In the United States alone, there are 38 million people with diabetes and a staggering 97.6 million with prediabetes. Diabetes is a metabolic disorder where the body loses the ability to regulate blood sugar levels. It occurs when the pancreas either does not produce enough insulin or the body cannot effectively use the insulin it produces. Diabetes is a chronic, life-changing condition. Daily life requires constant food-vigilance, blood-sugar testing, and usually involves injections of synthetic insulin to keep blood sugar at safe levels.
In the United States, diabetes is thought to cost around $400 billion every year. At the heart of all this is Type 2 diabetes (T2D), which represents up to 95% of all diabetes cases. T2D is characterized by insulin resistance, deterioration of pancreatic cell function, and impaired glucose production. T2D is a ticking time bomb, and when not treated properly, can have catastrophic health implications.
The problem is that, even though we do have effective treatment plans for diabetes, they are often poorly adhered to. This is mostly down to their demanding nature, which typically involves strict dieting and exercise, precise testing and scheduling, frequent medication adjustments, and unpleasant side effects.
Now, thanks to a breakthrough solution from biochemists at Stanford University, we have the hope of a simplified treatment — one that might ensure effective glycemic control. It could revolutionize T2D management.
The way things stand
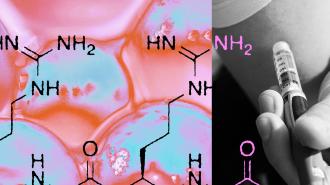
In a healthy person’s digestive tract, the body will produce certain hormones to regulate your blood sugar levels. These hormones control how much or how little energy to “let through” and how much to whisk away to other areas of the body for processing. For people with T2D, these hormones are either absent, inadequate, or overproduced. The one of the most effective kinds of diabetes medications, called glucagon-like peptide-1 receptor agonists (or GLP-1 RA for short), uses a synthetic hormone as a substitute. These GLP-1 RAs play a crucial role in lowering blood glucose levels by stimulating insulin and suppressing glucagon secretion.
Other than improving glucose control, GLP-1 RAs also help to reduce your appetite and body weight, and they are increasingly being used to help reduce obesity. Despite their effectiveness, GLP-1 RAs have side effects, and they face an additional challenge: they require a certain sustained level of the drug in your blood to be effective. Without those levels, GLP-1 RAs will be wildly unpredictable.
All of which means that the existing treatment regimens for those needing GLP-1 RAs involve daily or weekly injections (and anywhere in between). The frequency and burden of these treatments often hinder patient adherence, which makes treatment less effective. This sets up a need for a better drug delivery technology that makes it easier for diabetic patients.
The hydrogel and the rats
The team from Stanford University developed a groundbreaking hydrogel technology that allows for extended GLP-1 RA delivery. This hydrogel, made with biodegradable nanoparticles, can release GLP-1 RAs for up to four months with a single dose. This not only promises to reduce the frequency of injections, but it also helps to maintain the drug’s stability and efficacy over time.
Practically, the hydrogel is also a medical marvel; it has fewer manufacturing requirements, is easier to inject, and has rapid self-healing to prevent burst release. In other words, this hydrogel can, over months and with a single injection, do what dozens of injections currently do. It even does the job better.
The team tested the drug both in a test tube setting and by injecting rats. When under the microscope, the hydrogel was seen to retain up to 50% of its GLP-1 RA after two weeks, proving a gradual and steady release. When tested on rats, the studies likewise proved hopeful. Not only did it prove the drug was biocompatible (in that it didn’t harm the rats’ organs in any way), but it also reduced the diabetic rats’ blood glucose levels and managed their body weight. Finally, the study proved that the hydrogel treatments were more effective than compared with the daily 20 mg doses used as a control, which is to say, this looks much better than existing therapies.
A new era
The development of hydrogel-based GLP-1 RA medication would represent a fairly major advance in diabetes management. It could improve patient adherence and treatment outcomes in T2D, saving thousands of lives and millions of dollars. Figuring out exactly how well it works in larger animals, like humans, is the next step to eliminating dozens or hundreds of shots for patients every year.
Looking ahead, this technology could be a game-changer, transforming the landscape of diabetes treatment. It also has the potential to aid in obesity management in a way that more people might find bearable. As these hydrogel formulations move closer to clinical application, they offer a beacon of hope for millions battling T2D, heralding a new era of simplified, effective diabetes care.