Pain makes it hard to sleep, and poor sleep worsens pain. One affliction feeds the other to create a vicious cycle. That, in turn, can worsen the many coexisting conditions of sleep deficiency, including stress, fatigue, anxiety, depression, and a reduced immune response. It’s a problem likely familiar to the one-third of U.S. adults who report a sleep disorder or inadequate sleep.
Unfortunately, health professionals don’t understand the underlying mechanisms perpetuating this cycle. Many systems throughout the body play a part in both circadian rhythm and pain response, including the pineal gland, the immune system, and parts of the central nervous system separate from the brain. The problem is a medical mystery, a complicated “whodunit?” where no one stands out as the main suspect.
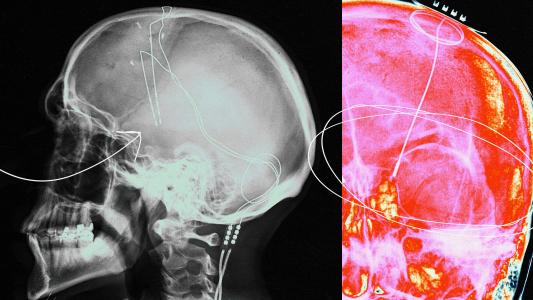
A new study led by researchers from the Massachusetts General Research Institute, however, may have discovered an important clue in the thalamus, specifically a part called the “thalamic reticular nucleus.” It’s a relay center that sends data to the outermost layers of the brain through a network of nerve fibers, and it plays pivotal roles in the sleep-wake cycle, directing attention, and how we process sensory information, like pain.
For these reasons, the researchers hypothesized that it could help us to understand pain sensitivity from disrupted sleep. And their findings suggest a possible way to one day ease, or even break, the cycle.
More than just beauty rest
To test their hypothesis, the researchers brought mice into the lab and deprived them of sleep between 7 a.m. and 1 p.m. daily for five days straight. The mice were kept awake by occasional raps on the pen or introducing new objects for them to explore. The mice then underwent a series of behavioral tests before being allowed to rest for the day.
Like humans, mice undergo various sleep cycles (specifically REM and non-REM sleep). But unlike humans, mice nod off intermittently for an average of 12 hours a day. In other words, that 7-to-1 schedule, which seems like a short workday to us, is the mousey equivalent of pulling an all-nighter after your day job.

For the behavioral tests, the researchers would poke the mice or heat up a section of the pen floor to see how quickly the mice would move away. They found that the sleep-deprived mice were far more sensitive to these irritations and withdrew much quicker. These results matched self-reports in humans showing that sleep disruption led to higher pain scores and more sensitivity.
The researchers then analyzed the metabolites in the mice’s brains, specifically in the thalamic reticular nucleus. Sleep-deprived mice had lower levels of a neurotransmitter known as NADA.
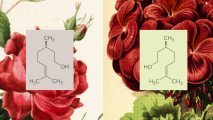
NADA belongs to a family of neurotransmitters that activate receptors of the body’s endocannabinoid system. This cell-signaling system was only discovered in 1988, and research into it remains relatively new. But that research suggests the system plays an important role in many moment-to-moment bodily functions as diverse as metabolism, immune response, and — most important for our purposes — sleep and pain regulation.
(And yes, the word endocannabinoid does look similar to cannabis. That’s no coincidence. Endocannabinoid molecules like NADA have structures similar to those found in the cannabis plant. The psychoactive compounds in cannabis work by hijacking this system.)
Without NADA, the cannabinoid receptors of the thalamic reticular nucleus weren’t as active and that seemed to have an effect on controlling pain perception. To test this, the researchers administered NADA into the mice’s brains through a microinjection. The mice who received this injection saw their pain sensitivity return to normal. This result suggests that both the production of NADA and the activation of the cannabinoid receptors are important for reducing pain sensitivity after sleep deprivation.
[T]he endocannabinoid system might break the vicious cycle between pain and sleep loss.
Shiqian Shen
“We provide a mechanism as to how sleep disruption leads to exaggerated pain, suggesting that harnessing the endocannabinoid system might break the vicious cycle between pain and sleep loss,” Shiqian Shen, the clinical director of Massachusetts General Hospital’s Tele Pain Program and the study’s co-senior author, said.
The study was published in Nature Communications, an open-access, peer-reviewed journal published by Nature Portfolio.
NADA enough research (yet)
Of course, the results of mice studies don’t necessarily translate to humans. They only hint at possibilities and areas where future studies may prove fruitful. Even so, the researchers note that their findings are part of a growing body of research into the endocannabinoid system.
In the study, they point to several pharmacological studies showing NADA to have properties that enhance the transmission of pain signals in the nervous system, as well as inhibiting them. They also note that endocannabinoids like NADA have been implicated in many neurological disorders such as epilepsy, Parkinson’s, and Alzheimer’s.
The culmination of this research suggests that research into the physiological roles of NADA — which the researchers point out is largely lacking at the moment — could open routes to new therapeutic strategies for helping to break the pain-sleep cycle as well as other neurological disorders.