Transplanting lab-grown dopamine neurons into the brains of people with Parkinson’s diseases appears to reduce their symptoms — suggesting that stem cells could be the key to ending the devastating disease.
The challenge: Parkinson’s is a progressive neurological disorder thought to be caused by the loss of brain cells that make dopamine, a chemical that helps neurons communicate.
By the time a person is diagnosed, they’ve typically already lost 50-80% of their dopamine-producing neurons. This leads to irregular brain activity and the disease’s characteristic movement issues, such as tremors, stiffness, and impaired coordination.
While drugs can supplement dopamine in the brain (most famously L-DOPA) or cause remaining healthy dopamine neurons to increase their output, there’s currently no way to repair damaged neurons or stop the progression of the disease.
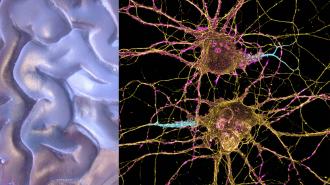
New dopamine neurons: Several research groups are hopeful that stem cells — which are capable of developing into any kind of cell — could give doctors a way to replenish Parkinson’s patients’ dwindling supply of dopamine neurons.
BlueRock Therapeutics, a subsidiary of pharma giant Bayer AG, is one of those groups.
On August 28, the company reported that its in-development stem cell therapy, called “bemdaneprocel” (BRT-DA01), increased the amount of time participants were free of Parkinson’s symptoms each day. The treatment was also found to be safe and tolerable by patients.
“While this is a small open-label study, meeting the study’s primary objective for safety and tolerability along with initial improvements seen in clinical outcomes represents a great step forward,” said Claire Henchcliffe, one of the study’s principal investigators.
The trial: The team at BlueRock first extracted stem cells from donated embryos. After coaxing the cells into developing into dopamine neurons, they implanted either a high or low dose of them in the brains of 12 trial participants.
The safety and tolerability of the treatment was studied over the following year, during which time the participants also received immunosuppressants to reduce the likelihood of their bodies rejecting the lab-grown neurons.
High-dose patients reported an increase of 2.16 hours each day that their symptoms were well-controlled.
No serious adverse events related to the drug were reported during the year of follow-up, and the researchers say they saw evidence in PET scans that the dopamine neurons survived and were incorporated into the patient’s brains.
Prior to the surgery, participants recorded how many waking hours each day their symptoms were well-controlled or not.
One year after treatment, high-dose patients reported an increase of 2.16 hours each day that their symptoms were well-controlled. The low-dose group saw an average improvement of 0.72 hours.
Looking ahead: BlueRock presented data from the trial at the International Congress of Parkinson’s Disease and Movement Disorders, but it has yet to publish the data — that might not happen until it finishes the planned second year of follow up with participants.
In the meantime, the company is already planning a phase 2 trial that’s expected to begin in the first half of 2024. It will test the lab-grown dopamine neurons in a larger group of people, with a focus on determining whether they can actually replace those lost to Parkinson’s.
“The standard of care for millions of people living with Parkinson’s disease has only marginally improved in the past decades, and the existing unmet medical need will only become higher due to the growing aging population,” said Christian Rommel, head of R&D at Bayer.
“The positive outcome of this Phase I clinical trial is a clear step forward, and it brings us closer to delivering new treatment options to patients,” he continued.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].