A new stem cell therapy for Parkinson’s disease has just been administered to a person for the first time — and if it works as hoped, it could revolutionize how doctors treat the disease.
“[W]e maybe have a treatment that we can offer to patients…in the beginning of the disease, like a one time treatment, and that will last for the rest of the patient’s life and make it possible to reduce the medication that patients otherwise need,” said principal investigator Gesine Paul-Visse from Sweden’s Lund University.
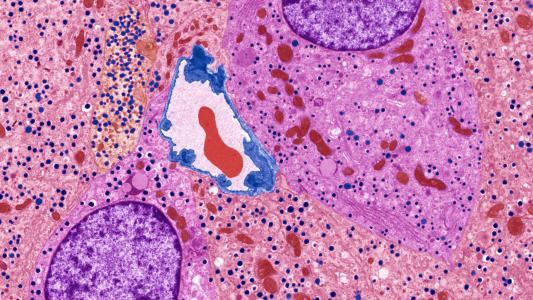
The challenge: An estimated 8.5 million people are living with Parkinson’s, a progressive neurodegenerative disorder caused by the loss of the brain neurons that produce the chemical dopamine, which helps coordinate movement.
The shortage of dopamine leads to the hallmark symptoms of Parkinson’s, including tremors, stiffness, and impaired coordination. Medications can increase dopamine levels, but they can also cause side effects, interfere with other meds, and become less effective over time.
“The use of stem cells will, in theory, enable us to make unlimited amounts of dopamine neurons.”
Roger Barker
The idea: Rather than relying on meds, Paul-Visse and her collaborators in Sweden and the UK hope to actually replace dopamine-producing nerve cells in the brains of Parkinson’s patients using embryonic stem cells, which can develop into almost any type of cell in the body.
For their therapy, STEM-PD, the researchers programmed stem cells sourced from donated embryos to turn into dopamine nerve cells. When transplanted into the brains of rodent models of Parkinson’s, the cells developed as hoped, and the animals’ motor symptoms were reversed.
The researchers have now administered the treatment to a person for the first time, and by the end of their newly launched STEM-PD trial, eight people with moderate Parkinson’s will undergo the therapy.
Looking ahead: The trial’s primary goal is to assess the safety of STEM-PD, but the researchers will also be looking to see if the therapy improves symptoms, reduces the need for medication, or leads to the development of new dopamine-producing neurons in the brain.
The efficacy of the treatment won’t be apparent right away, though.
“These cells that we are transplanting are actually immature, so they need some time to mature in the adult brain, and that will take at least a year, maybe even longer,” said Paul-Visse. “So we won’t expect to see any changes before in one year’s time.”
The big picture: Treatments that work in animals often don’t translate to people, but if STEM-PD proves safe and effective, the impact could be huge, given that stem cells can be duplicated an unlimited number of times.
“The use of stem cells will, in theory, enable us to make unlimited amounts of dopamine neurons and thus opens the prospect of producing this therapy to a wide patient population,” said clinical lead Roger Barker from the University of Cambridge. “This could transform the way we treat Parkinson’s disease.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].