Johns Hopkins University (JHU) researchers have developed an experimental brain cancer treatment that not only cured 100% of mice that received it, but also trained their immune systems to fight future cancers.
The challenge: Glioblastoma is a rare but aggressive type of brain cancer — only 5% of patients live for more than five years after they’re diagnosed, and the average survival time is just 12-18 months. It is considered the deadliest kind of cancer.
The standard glioblastoma treatment regimen starts with surgery to remove as much of the tumor as possible. After that, patients typically undergo chemo or radiation therapy to kill lingering cells.
While this approach can buy patients some time, it’s almost impossible to kill every cancer cell, and as a result, glioblastoma almost always recurs.
Glioblastoma is considered the deadliest kind of cancer.
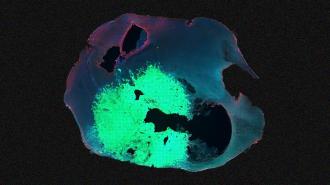
What’s new? The new brain cancer treatment developed at JHU is a hydrogel that’s applied to the space left in the brain after a glioblastoma tumor has been surgically removed.
In the gel are nano-sized threads of paclitaxel, an existing, FDA-approved chemotherapy drug used to treat certain cancers outside the brain.
These threads serve as delivery vehicles for patients an antibody that binds to CD47, a protein that cancer cells make to avoid being attacked by white blood cells called “macrophages.” When the antibody sticks to cancer cells, it interferes with that protection and lets the macrophages target the cancer.
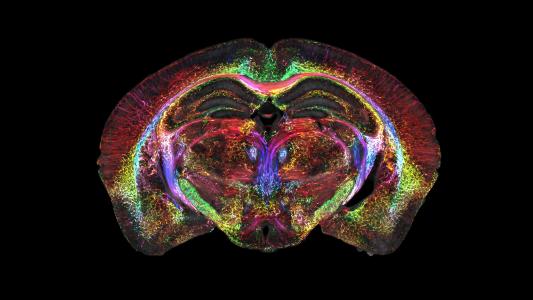
The study: To test the experimental brain cancer treatment, the researchers implanted brain tumors in mice and then divided them into six groups of eight mice.
Mice in one group didn’t have their tumors removed — they died a median of 22 days after tumor implantation. Mice in another group had their tumors surgically removed eight days after implantation — those survived a median of just 28.5 days.
Two other groups of mice were treated with a hydrogel containing either only the antibody or only paclitaxel, after having their tumors removed — mice in those groups survived a median of 39 and 63 days.
“This hydrogel combines both chemotherapy and immunotherapy intracranially.”
Betty Tyler
Another group of mice got a hydrogel containing both the chemo drug and the antibody, but didn’t have their tumors removed first. Half of those mice managed to survive for 80 days — long enough to be considered “long-term survivors.”
A final group was treated with the combined antibody plus chemo hydrogel after tumor-removal surgery. All of those mice lived at least 80 days and showed no signs of recurrence. Side effects were minimal, at least as far as researchers can observe in mice.
“This hydrogel combines both chemotherapy and immunotherapy intracranially,” said co-author Betty Tyler. “The gel is implanted at the time of tumor resection, which makes it work really well.”
Take two: The new brain cancer treatment seems to do more than just kill cancer cells missed during surgery, too.
On day 80 after the initial tumor implantation, the researchers rechallenged any surviving mice with tumor cells. When they checked those rodents again 20 days later, they could find no signs of cancer in the brains of those that had been treated with the fully loaded hydrogel.
“These results strongly substantiate that a robust and durable antitumor memory immune response was established by a single localized … hydrogel treatment,” the researchers write.
“We don’t usually see 100% survival in mouse models of this disease.”
Betty Tyler
Looking ahead: Given that only half of the mice that didn’t have their tumors removed before treatment survived the full 80 days, it doesn’t seem like JHU’s new hydrogel could eliminate the need for surgery.
Still, if the results of the mouse study translate even somewhat to humans — always a big if — the hydrogel could provide new hope for people with this deadly disease.
“We don’t usually see 100% survival in mouse models of this disease,” Tyler said. “Thinking that there is potential for this new hydrogel combination to change that survival curve for glioblastoma patients is very exciting.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].