A new device that can simulate up to eight organs at once could be a huge boon to drug development, helping researchers better understand diseases and identify meds that are most likely to be safe and effective in human trials.
“This is the closest thing we can do to recreate the human body, outside the human body,” Hannes Campo, first author of a paper on the device, told WGNTV.
The challenge: Drug development starts with learning everything we can about a disease, including where it starts, how it spreads, and what drug compounds could potentially stop it.
“This is the closest thing we can do to recreate the human body, outside the human body.”
Hannes Campo
Once researchers have come up with a game plan for treating the disease, they experiment in the lab on samples of human cells and then animal models. If a treatment appears safe and effective in those tests, it could move on to clinical trials.
But this process for screening whether drugs will work in people isn’t reliable — only 10% of those that make it into clinical trials ever reach the market. Most drugs fail because they simply don’t work or cause intolerable side effects, leading to huge losses of time and money.
“It’s one more fail-safe check before we put them in bodies.”
Julie Kim
Extra step: Scientists at Northwestern University have developed a device, called Lattice, that they believe could reduce the number of destined-to-fail clinical trials, making drug development faster, safer, and more efficient.
“There’s nothing in between animal testing and human clinical trials, and we find that many drugs fail in humans,” said lead scientist Julie Kim.
“Lattice could be that intermediate step between animal studies and clinical trials, because we can test drugs that have passed animal studies to see if they’re safe for human tissues,” she continued. “It’s one more fail-safe check before we put them in bodies.”
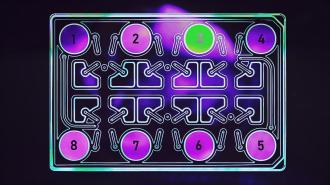
Wells: Lattice is about the size of a small shoebox, and it contains eight wells that are filled with simulated blood (or “media”). The wells are connected by channels that can be opened or closed by a computer, allowing media to flow from one well to another.
Researchers can put anything they like in the wells — tissue samples, diseased cells, candidate drugs, etc. — and then move the media between them to study interactions.
“If you know that the liver metabolizes the drug, you want to know whether those metabolites are safe or not in the human, and so we would put a liver [sample] in [Lattice] along with some of the other tissues,” Kim told WGNTV.
The media can keep the tissue samples alive for up to 28 days, which is longer than they would survive in a petri dish, according to Kim. Her team is currently working to extend the timeframe even further.
“We wanted to make it as easy as using a smartphone — take it out of the box, turn it on, and use it.”
Julie Kim
Disease simulator: Lattice could be used in the earliest stages of drug development, too, when researchers are still trying to understand a disease and how it spreads.
“When something’s happening in the body, we don’t know exactly who’s talking to whom,” said Kim. “Currently, scientists use dishes that have one or two cell types, and then do in-depth research and analysis, but Lattice provides a huge advancement.”
“This platform is much better suited to mimic what’s happening in the body, because it can simulate so many organs at once,” she continued.
Looking ahead: Kim’s lab is currently using Lattice to study polycystic ovarian syndrome (PCOS), an incurable hormonal disorder that’s a leading cause of infertility. She says she’s hopeful the device will be used broadly in the research and pharmaceutical fields.
“[W]e wanted to make something user friendly, so you don’t need engineers on hand to assemble or troubleshoot it,” said Kim. “We wanted to make it as easy as using a smartphone — take it out of the box, turn it on, and use it — so researchers can get data and not spend too much time on how to work it in their lab.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].