This article is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.
Managing your health often means being a slave to medication.
People with diabetes, for example, typically need to inject themselves with insulin at precisely the right time, multiple times a day, to keep their condition in check. Cancer patients, meanwhile, might have to visit a clinic three times a week for drug infusions to put the disease in remission.
Add in the high cost of medications, confusion surrounding how they’re supposed to be taken, and other factors, and you end up with an estimated 50% of patients not taking their meds as prescribed, a phenomenon called “nonadherence.”
In the US, medication nonadherence is associated with 125,000 deaths, at least 10% of all hospitalizations, and $100 billion in avoidable spending annually, but in the future, “living pharmacies” could make it far easier — and cheaper — for people to get the meds they need, right when they need them, all the time.
Living pharmacies
The idea behind a “living pharmacy” is that we can put living cells in an implantable device, and those cells could then be triggered to release a therapeutic biomolecule, such as the hormone insulin or a cancer-fighting protein, on demand.
While cells can’t be programmed to make all the meds we use, biotherapeutics are a quickly growing field of pharmacology, with medications approved to treat a wide variety of illnesses.
“No need to carry drugs, no need to inject therapeutics and — depending on how long we can make the device last — no need to refill the device.”
Jonathan Rivnay
Living pharmacies aren’t to be confused with implants that are loaded with drugs before insertion, like Nexplanon, which releases the hormone progestogen to prevent pregnancy, or Vantas, which releases a medication that helps fight prostate cancer.
Those devices have to be replaced when they run out of their medication — a living pharmacy is designed to create its own drugs, indefinitely.
Resetting the clock
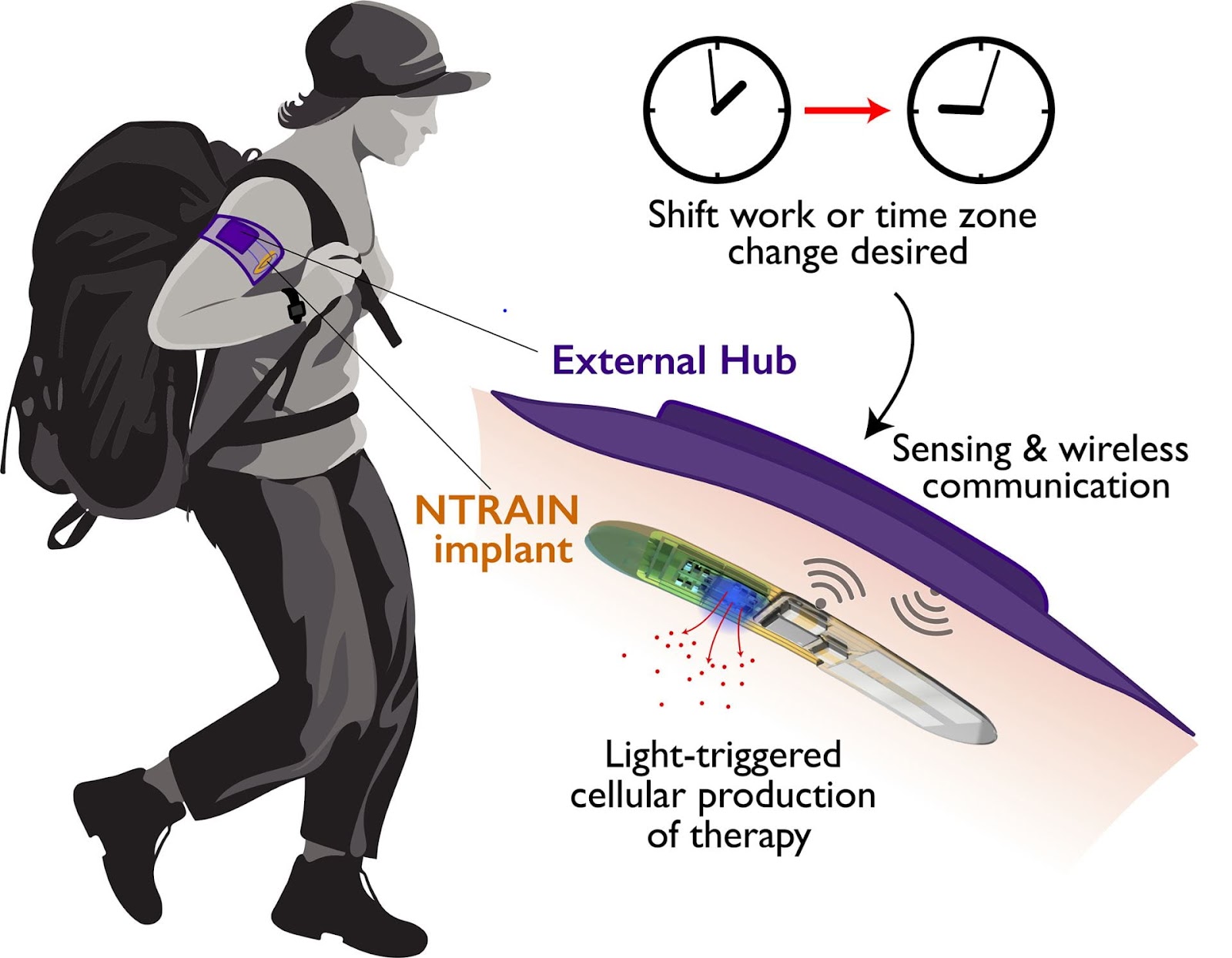
Living pharmacies don’t actually exist yet, but in 2021, DARPA awarded a Northwestern University-led team $33 million to develop one to control the body’s circadian clock. The idea is that it could help soldiers quickly overcome jet lag or adapt to changes in their work schedules.
The microchip implant they’re developing — NTRAIN (Normalizing Timing of Rhythms Across Internal Networks of Circadian Clocks) — contains cells engineered to release the same peptides that naturally control our circadian clock when triggered by a light on the implant.
The whole thing is placed under the skin of the arm, and a wearable armband connected to a smartphone app is used to wirelessly turn it on or off.
“No need to carry drugs, no need to inject therapeutics and — depending on how long we can make the device last — no need to refill the device,” said co-principal investigator Jonathan Rivnay. “It’s like an implantable pharmacy on a chip that never runs out.”
Developing NTRAIN — or any living pharmacy — won’t be easy.
The whole thing needs to be biocompatible, and the engineered cells need to be protected from the immune system, while still being provided with everything they need to live — otherwise, they’ll die off, and the tech will stop working.
The NTRAIN team plans to house its cells within a special membrane that lets nutrients in, but keeps immune cells out. Just in case something does cause the cells to stop working as designed, they’re also developing a pill that a person could take to deliberately kill them.
In an August 2023 update, Rivnay said the team is currently working on an “on-site oxygenator” to provide the cells with the oxygen they need to stay “healthy and happy.” It extracts this oxygen from water in the body and has already produced promising results when tested in vivo (though the researchers didn’t say in what species).
“The real innovation here is being able to produce drugs inside the patient.”
Omid Veiseh
In-human studies of the NTRAIN device are expected to begin in 2025, and even though the implant is being developed for the military initially, everyone could eventually benefit.
The team notes the potential for NTRAIN to help first responders and other shift workers adapt to their changing schedules, and the tech could also be tweaked to create other therapeutic biomolecules.
“Sleep control is something we can track while we develop this implant, but the real innovation here is being able to produce drugs inside the patient,” said co-principal investigator Omid Veiseh from Rice University.
“If we can bring all of that manufacturing right into the patient and produce high-quality compounds on an as-needed basis, the possibilities are infinite,” he continued.
“REACT will create new devices to improve a person’s ability to get the medicine when and where they need it.”
Paul Sheehan
Looking ahead
We might not have to wait for the NTRAIN team to finish developing its device to start seeing living pharmacies used in patients — insulin-releasing implants developed at MIT and ETH Zurich have already shown promise in studies of diabetic mice.
The US government is ready to start funding development into more of the devices, too.
On September 29, the Advanced Research Projects Agency for Health (ARPA-H) announced the launch of a new program called REACT (Resilient Extended Automatic Cell Therapies). As part of it, ARPA-H will fund research into living pharmacies, which it hopes will make adhering to a medication schedule both easier and more affordable for patients.
While the announcement notes the potential for living pharmacies to help people combating cancer, diabetes, and obesity, the program isn’t limited to any particular conditions, and ARPA-H expects to provide funding to multiple groups, with the amount depending on the quality of proposals and how many it receives.
“For many people living with acute and lifelong diseases, complex care navigation demands, including consistently taking the right dose at the right time, can dramatically undermine their health,” said Paul Sheehan, REACT’s program manager at ARPA-H.
“REACT will create new devices to improve a person’s ability to get the medicine when and where they need it … providing them with more control and freedom in their daily lives and improving their well-being,” he continued.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].






