This article is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.
Scientists at the University of Minnesota (UMN) have found a way to rewarm cryogenically frozen rat kidneys so that they could be successfully transplanted into new rodents up to 100 days later — a world’s first achievement that could revolutionize organ transplantation.
“This is the first time anyone has published a robust protocol for long-term storage, rewarming, and successful transplantation of a functional preserved organ in an animal,” said co-senior author John Bischof.
“All of our research over more than a decade and that of our colleagues in the field has shown that this process should work, then that it could work, but now we’ve shown that it actually does work,” he continued.
The challenge: In 1954, surgeons in Boston made history by performing the first successful organ transplant, placing a healthy kidney donated by 23-year-old Ronald Herrick into the body of his twin brother, Richard, who was dying of kidney disease.
Since then, US surgeons have completed more than 1 million organ transplants, and thanks to advances in surgical techniques, immunosuppression, and more, the vast majority performed today are successful, adding years onto the lives of recipients.
Once removed from a donor, organs are only considered viable for so long.
Unfortunately, not everyone who needs a new organ gets one — 17 people on the US waiting list die every day because an organ wasn’t available to them in time.
This is largely a problem of supply — there simply aren’t enough compatible donor organs to go around — but the number of deaths could potentially be lower if the organs that are available always went to those most in need of them.
That isn’t currently the case because, once removed from a donor, organs are only viable for so long. Hearts and lungs must be transplanted within 4 hours of removal, for example, while kidneys can last up to 48 hours — the longest of any major organ.
The need to use organs so soon after they’re removed means geography and luck plays a role in who gets donor organs — typically, priority for hearts goes to recipients within a 250-mile radius of the donor’s hospital, even if there’s a sicker patient who’s an equally good match just outside that radius.
Even if the person most in need of an organ is chosen to receive it, the slightest setback in getting the organ to the patient — due to a delayed flight, for example — can mean the surgery must be canceled and the life-saving organ discarded.
More lead time before transplant surgeries could improve patient outcomes.
The short windows of viability can also reduce the odds of success for a transplant surgery.
Because kidneys can come from living donors, doctors will sometimes wait to remove them until after they’ve transplanted stem cells from the donor into the recipient. Stem cells can help prepare the body to accept the new organ and reduce (or even eliminate) the need for immunosuppressive drugs, which leave patients susceptible to infections.
If doctors had more than a few hours notice that a patient would be receiving a heart, lung, or other organ from a certain donor, they might be able to do the same thing before those surgeries.
The idea: Cryopreservation — cooling and storing biological tissues until we want to use them — has long been considered as a way to extend the viability of donor organs, but simply placing organs in freezers isn’t an option: as the water in the organ turns to ice, it expands and creates sharp crystals that damage the tissue.
In the 1980s, scientists discovered that they could cryopreserve human egg cells without causing ice crystals to form if they first treated the eggs with chemicals called “cryoprotectants” and then immersed them in liquid nitrogen to rapidly freeze them. The eggs could then be warmed later and used for IVF.
This process, called “vitrification,” has since been explored in depth as a way to preserve organs, but researchers kept running into the problem of ice crystals forming during the rewarming phase, due to some parts of the organ heating up faster than others.
What’s new? The UMN team appears to have found a way to overcome this issue.
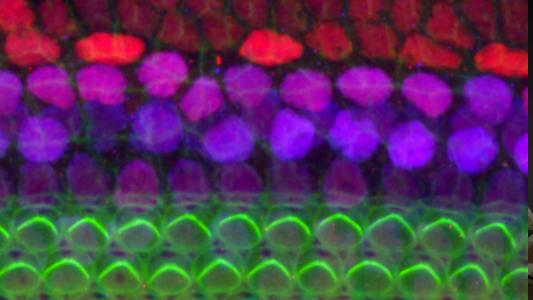
In their study, published in Nature Communications, they mixed iron oxide nanoparticles into a cryoprotectant solution before pumping it through the blood vessels of kidneys removed from rats. They then cooled the organs to -122 °C (-187.6 °F) and stored them for up to 100 days.
“They were fully functioning kidneys that were completely indistinguishable from transplants of a fresh organ.”
Erik Finger
When it was time to rewarm the cryogenically frozen organs, the researchers placed them inside a copper coil and ran a current through it to create a magnetic field. This magnetic field caused the iron nanoparticles inside the kidneys to heat up, warming the organs evenly in just 90 seconds.
After this “nanowarming,” the scientists flushed the cryoprotectant and nanoparticles from the kidneys and transplanted them into five rats.
“During the first two to three weeks, the kidneys weren’t at full function, but by three weeks, they recovered,” said co-senior author Erik Finger. “By one month, they were fully functioning kidneys that were completely indistinguishable from transplants of a fresh organ.”
Looking ahead: The cryogenically frozen organs did not perform as well initially as fresh kidneys would have — it took 45 minutes for them to begin producing urine, as opposed to the few minutes expected of a kidney that didn’t undergo the vitrification process.
The fact that they eventually started functioning properly is encouraging, but it’s unknown whether they’d have the same lifespan as traditional donor kidneys — the rats were all sacrificed for analysis 30 days after the surgery.
Then there’s the caveat that accompanies all rodent studies: results often don’t translate to people.

The UMN team told Science Magazine that it sees “no physical reason” its nanowarming process wouldn’t work on larger cryogenically frozen organs. They’re already experimenting with pig kidneys, and testing on human organs could be just a year or two away.
Clinical trials in which organs are actually transplanted into people could potentially start five years after that, the researchers told STAT News, but such studies are notoriously difficult to conduct given the limited supply of donor organs.
Finding donors willing to have their organs frozen and later rewarmed — rather than just given to people in need right away — could prove particularly challenging, and doctors and patients might not want those organs if there’s any possibility a fresh one could come along in time.
The big picture: If the UMN team is able to clear those hurdles, the ability to store organs seemingly indefinitely could ensure the people most in need are always at the top of the list when a matching donor organ becomes available, regardless of where they live.
This would undoubtedly improve the donation system, but it wouldn’t overcome the core problem of too few donor organs to begin with.
In an attempt to address that issue, other researchers are creating organs in labs, growing human organs in animals, and even transplanting animal organs into people. If those projects can end the organ shortage, they could be combined with UMN’s storage tech to ensure a matching organ is available for anyone, anywhere, anytime.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].