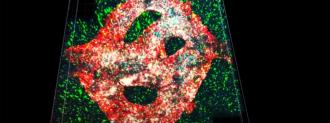
In a cool-but-kind-of-freaky first, researchers at Tel Aviv University have 3D-printed an active tumor.
Grown from cells plucked from patients off the operating tables of Tel Aviv Sourasky Medical Center, they bioprinted a glioblastoma tumor — an especially brutal brain cancer.
“Glioblastoma is the most lethal cancer of the central nervous system, accounting for most brain malignancies,” Ronit Satchi-Fainaro, director of the Cancer Biology Research Center and the study leader, said.
The researchers hope that having a functioning glioblastoma tumor could help researchers better understand them, allowing them to discover drugs and craft the most effective therapies. And one day, we may be able to design a cancer treatment plan tested first on your specific cancer.
If they can take a sample of your glioblastoma, as well as the cells around it, they could 3D-bioprint “100 tiny tumors and test many different drugs in various combinations to discover the optimal treatment for this specific tumor,” Satchi-Fainaro said.
A plastic dish isn’t you: As exciting as scientific discoveries in a dish can be, they aren’t always representative of what happens in your body. Satchi-Fainaro and her team had that difference made quite clear while studying glioblastoma.
They had discovered that glioblastoma tumors release a special protein that messes with immune system cells in the brain; rather than attacking the tumor, they actually help it, allowing the cancer to spread.
Grown from cells plucked from patients off the operating table, researchers bioprinted a glioblastoma tumor — an especially brutal brain cancer.
But to find this out, they needed to use real, surgically removed tumors, not the 2D tumor cells grown in lab dishes.
“The reason is that cancer, like all tissues, behaves very differently on a plastic surface than it does in the human body,” Satchi-Fainaro said. “Approximately 90% of all experimental drugs fail at the clinical stage because the success achieved in the lab is not reproduced in patients.”
Reproducing the patients: This is where a 3D-printed, active glioblastoma tumor may come into play.
The glioblastoma tumor, published in Science Advances, is made of a gel material that is meant to simulate the tissues of the brain, 3D Printing Industry reported. It’s laced with a series of tubes that can become a model blood vessel system, allowing the team to not only 3D-print the glioblastoma tumor, but a representation of the body’s environment around it.
“Approximately 90% of all experimental drugs fail at the clinical stage because the success achieved in the lab is not reproduced in patients.”
Ronit Satchi-Fainaro
“Our 3D engineered tissue constructs are based on two bioinks, a tumor bioink and a vascular bioink,” the researchers wrote; in other words, you’ve got your tumor ingredients, you’ve got your blood cell ingredients, and you 3D-print both to get to the active glioblastoma tumor.
Once the tumor has been 3D-printed, the patient’s blood is pumped through the tumor, Reuters reported, followed by the drug or therapy you want to test.
Microenvironmental crisis: Modeling the area around the glioblastoma — called the “tumor microenvironment” — is especially important because it makes a big difference to the tumor’s defense systems— like, say, snowing the immune system.
Because the tumor’s tricks on the tissues around it are so crucial, “models that better mimic the intricate microenvironment [of glioblastoma] have the potential to facilitate the development of effective alternative treatment options,” the team wrote.
One day, we may be able to design a cancer treatment plan tested first on your specific cancer’s tumors.
Once printed, their active glioblastoma tumor could then be used to simulate therapies, identify drug targets, and test new drugs.
“We have about two weeks (to) test all the different therapies that we would like to evaluate (on) that specific tumour, and get back with an answer – which treatment is predicted to be the best fit,” Satchi-Fainaro told Reuters.
If their model tumor reacts, then the real one may as well.
Eventually, the researchers hope that their tumors may be used as personalized medicine — test drugs and therapies, or find weaknesses in, your tumor and microenvironment, then put together a plan of attack before taking it to the cancer.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].