While a cure is still nowhere in sight, the Alzheimer’s field is at a pivotal juncture, which is driving renewed appetite for future research.
The recent historic approval of a treatment to slow down Alzheimer’s, combined with a better understanding of the disease, is solidifying the scientific consensus that a single, unicorn “cure” is unlikely to materialize for this complex disease.
Rather, the “holy grail” solution may be a drug cocktail, personalized to individual patients.
What is Alzheimer’s disease, and why is it so hard to treat?
Alzheimer’s disease (AD) is the most common form of dementia, impairing thought and memory to a degree that severely impacts daily living. As damage to the brain accumulates, AD becomes disabling and eventually deadly. Around 6.7 million Americans are living with AD, and one of its most troubling traits is that its damage can start decades before first symptoms appear.
This makes it very challenging to study. Even when symptoms do appear, they can show up very differently in different patients.
In the last five years alone, nine beta-amyloid targeting drugs failed phase 3 trials.
“It’s a fatal neurodegenerative disease that has a heterogeneous presentation, and initial diagnoses have historically had a 10-30% error rate,” said Dr Percy Griffin, the director of Scientific Engagement for the Alzheimer’s Association.
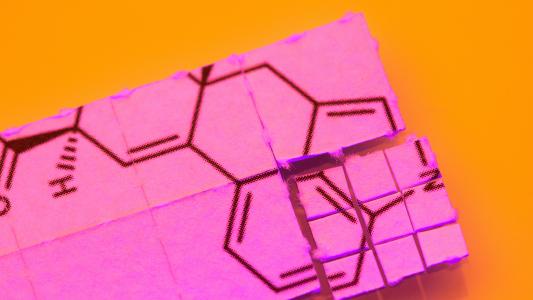
While much about the disease onset remains a mystery, the buildup of certain proteins in the brain has been linked to the impairing of neurons — nerve cells responsible for memory, language, behavior. As the disease progresses, beta-amyloid proteins accumulate into sticky plaques around neurons, while tau proteins appear as “tangles” inside neurons.
A long road for Team Amyloid
A good 30 years of research has been focused on drugs to clear beta-amyloid, but even with a very promising drug, success only comes after the near-perfect execution of a clinical trial. In the last five years alone, nine beta-amyloid targeting drugs failed phase 3 trials.
Many companies have shied away from investing in AD drugs due to the disease’s unique complications, including a heterogeneous population (varying rates of disease progression and symptoms), difficulties getting drugs to cross the blood-brain barrier (BBB), and testing a drug in an older population with other concurrent illnesses, according to Dr Sara Imarisio, Head of Strategic Initiatives, Alzheimer’s Research UK.
In 2021, US biotech company Biogen had a false start with the FDA’s accelerated approval of its monoclonal antibody (mAb) Aduhelm, which aims to clear beta-amyloid plaques. But the drug came under fire for its debatable efficacy and hefty price tag. Medicare declined to pay for it outside of clinical trials, leaving it largely unused.
“You can intervene in [Alzheimer’s] disease progression by knocking down levels of beta-amyloid.”
Graig Suvannavejh
However, earlier this year, Japanese company Eisai, in partnership with Biogen (getting a second chance), received controversy-free accelerated approval for Leqembi (lecanemab) — another amyloid-targeting antibody. A clinical trial showed it slowed the decline in cognitive function by 27% compared to placebo after 18 months.
A full-fledged approval — which will allow broader coverage by health insurance providers — is due this July.
“While Leqembi’s performance was modest at best, it gives us a better assurance that you can intervene in disease progression by knocking down levels of beta-amyloid,” said Dr Graig Suvannavejh PhD, Managing Director and Senior Biotech Analyst at Mizuho Bank.
Eli Lilly has a similar drug called donanemab and phase 3 results are expected this fall.
“There is a lot of anticipation for donanemab’s results, as earlier data have shown an impressive reduction in amyloid plaque levels but full results are needed to comment,” said Griffin.
“Drugs often struggle to reach effective potency levels that outweigh the potentially harmful side-effects.”
Graig Suvannavejh
The major issue for current beta-amyloid targeting drugs is getting levels of the drug high enough in the brain and across the BBB without compromising on safety.
“These drugs trigger an infiltration of cells trying to combat the disease, but that also comes with the potential risks of cerebral edema (ARIA-E) that can lead to brain swelling,” said Suvannavejh.
“Only a small fraction of the original amount of the injectable mAb is able to cross the BBB, so drugs often struggle to reach effective potency levels that outweigh the potentially harmful side-effects,” Suvannavejh added. In particular, Biogen’s Aduhelm was scrutinized for not having a balanced risk/benefit profile.
Companies such as Roche and Voyager are working on “shuttle” technology to improve drug delivery across the BBB. Meanwhile, oral small molecule drugs have better potential to cross the BBB. Private US biotech Alzheon has an amyloid-targeting pill, ALZ-801, in phase 3 trials due to complete in mid-2024.
Alternative pathways for treatment
While eliminating beta-amyloid has now shown some meaningful (though not major) benefits, blocking a combination of pathways that lead to neuronal damage might be the optimal approach for patients.
“New clinical trials are reflecting new insight on the disease,” said Imarisio, who noted various combinations could serve as a form of personalized therapy for the heterogeneous patient group.
Let’s look at some of the alternative approaches garnering the most attention.
Boosting immunity
Right now, enhancing the brain’s immune system, specifically microglia — immune cells that clear debris around neurons — is getting the most buzz.
“There has been an explosion of studies offering a better understanding of a microglial receptor called TREM2 and now many companies are investing in drugs targeting TREM2 to enhance microglia proliferation,” said Imarisio.
“Just as companies have found success in cancer by modulating the immune system, companies including Alector, Denali, and Vigil Neuroscience believe that harnessing the power of the immune system can help patients with neurodegenerative diseases,” said Suvannavejh.
Alector/Abbvie’s AL002 is an injectable mAb in a mid-stage (phase 2) human trial, due to finish sometime in late 2023/early 2024. Denali/Takeda’s DNL919, is a mAb in an early-stage (phase 1) human trial due to complete in July 2023. Meanwhile, Vigil Neuroscience is working on a TREM2 targeting pill, which is still in the pre-clinical laboratory stages.
Clearing tau tangles
While the clearing of tau has been overshadowed by the focus on beta-amyloid, the approach remains valid. “The scientific thinking around this approach is evolving, specifically around optimal binding domains, which may yield better efficacy in clearing the tau tangles,” said Griffin.
“While early tau-based approaches have not led to success, there are still a handful of companies with drugs aimed at lowering and clearing the proteins that build up in the brain,” said Suvannavejh.
Companies in phase 2 trials include: Eli Lilly with its oral LY3372689, due for trial completion in June 2024; Johnson & Johnson with its injectable mAb, JNJ-63733657, due for completion in late 2025; and Roche/UCB with their injectable mAb bepranemab also due for completion in 2025.
Fixing metabolism
Other researchers believe that AD is best understood as a neuro-metabolic disease, and poor metabolism and dysfunctional lipid metabolism in the brain can lead to neurodegeneration.
“This kind of mimics what people see with diabetes in terms of insulin sensitivity,” said Griffin, noting work being funded by the Alzheimer’s Association from T3D therapeutics to see if the dysfunction around how the brain uses energy in AD can be fixed.
The company’s lead candidate T3D-959 is an oral drug in a phase 2 trial. In order to target neurodegeneration, the once-daily pill aims to regulate transcription of genes involved in glucose energy and lipid metabolism.
A bit further down the pipeline….
Reducing neuroInflammation (NLRP3)
While in much earlier research stages, experts noted interest around the NLRP3 inflammasome target. Inflammasomes are a multiprotein complex that play a crucial role in activating inflammatory responses and can be triggered by beta amyloid and tau. This can contribute to the development of chronic neuroinflammation, leading to neuronal loss and cognitive impairment. While much of the research around NLRP3 inhibitors in AD is limited to pre-clinical testing, NLRP3 is implicated in many other inflammatory diseases and some big pharma companies including Roche, Novartis and Novo Nordisk have invested in NLRP3 inhibitors.
Gene-editing/CRISPR
Gene-editing technology CRISPR has been seen as a potential miracle therapy for complex diseases, and its application is also being pursued in AD — though in the very early preclinical stages.
Griffin noted Martin Kampmann’s lab at University of California San Francisco is studying how CRISPR-Cas9 can change immune cells in the brain to get them back on track — a similar concept to immunomodulation targeting TREM2.
“While CRISPR is a technique that has shown some early promise in mice, delivery in humans is a lot more complex and it will take some time to refine this approach for AD patients,” said Imarisio.
Where does that leave patients now?
While initial access to Leqembi will likely be restricted, eligible patients will gradually be able to enjoy its benefits. But there is still a huge unmet need to help current patients deal with symptoms.
Suvannavejh noted several companies are working on drugs that address both agitation and psychosis associated with AD. Axsome Therapeutics and BioXcel Therapeutics have phase 3 candidates treating agitation, while Otsuka aims to expand the use of existing depression drug Rexulti for agitation. Karuna Therapeutics has a phase 2 drug for AD-related psychosis.
While we’re still a long way from seeing a disease-reversing drug cocktail, experts remain optimistic that more accurate and accessible diagnostic tools may help to refine and accelerate future clinical trials — priming them for much higher success rates. Narrowing down patient populations will be the key to ensure there are less failures along the way, they noted.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].