A new coating for medical devices could prevent hospital-acquired infections, potentially saving lives and helping in the fight against antibiotic resistance.
The challenge: The CDC estimates that 4% of people admitted to US hospitals acquire at least one infection during their stay. About two-thirds of these hospital-acquired infections are caused by medical devices, such as catheters, stents, and pacemakers.
Complications from hospital-acquired infections kill nearly 100,000 patients every year.
Usually, colonies of microbes form slimy “biofilms” on the surfaces of the devices and then release cells that cause infections throughout the body. Biofilms are highly resistant to antibiotics, so affected patients often have to be treated with the strongest meds available.
Antibiotic resistance: Complications from hospital-acquired infections kill nearly 100,000 patients every year, and the number would be a lot higher if not for antibiotics.
However, the more often we prescribe these meds, the more opportunities we give bacteria to evolve resistance to them, turning them into “superbugs.”
To avoid returning to an era in which even minor infections are potentially deadly, we need to use antibiotics far more carefully and come up with solutions to fight antibiotic resistance.
In lab tests, the coating reduced the growth of biofilms on common medical devices by 80% to 93%.
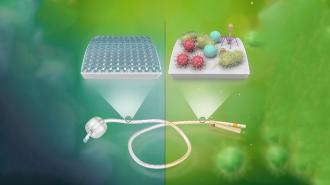
The idea: A UCLA-led team of researchers has now developed a coating for medical devices that could dramatically reduce the number of hospital-acquired infections — and the number of antibiotics needed to treat them.
“The beauty of this technology is that it can prevent or minimize the growth of biofilm without the use of antibiotics,” said senior author Richard Kaner. “It protects patients using medical devices — and therefore protects all of us — against microbial resistance and the proliferation of superbugs.”
How it works: UCLA’s coating contains molecules called “zwitterions,” which have an equal number of positive and negatively charged atoms. Once it’s sprayed onto a medical device, ultraviolet light is used to bind it to the item’s surface.
Zwitterionic materials are highly biocompatible and absorb water tightly — as a result, the treatment forms a hydration barrier on the device that prevents microbes from sticking to it.
“The beauty of this technology is that it can prevent or minimize the growth of biofilm without the use of antibiotics.”
Richard Kaner
In lab tests, the coating reduced the growth of biofilms on common medical devices by 80% to 93%. When 16 long-term urinary catheter users switched to devices coated in it, 10 said their urinary tract condition was “much better” or “very much better” than before.
“[One patient’s] previous catheters would become blocked after four days or so — she was in pain and needed repeated medical procedures to replace them,” Kaner said. “With our surface treatment, she now comes in every three weeks, and her catheters work perfectly without encrustation or occlusion — a common occurrence with her previous ones.”
Looking ahead: UCLA isn’t alone in trying to prevent hospital-acquired infections with clever coatings on medical devices, but according to Kaner, his team’s treatment is relatively low cost compared to current options.
A company spun out of his lab, SILQ Technologies, is now working to commercialize the coating, and the catheters used for the UCLA trial, which were cleared by the FDA in 2020, are its first product.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].