Researchers have used stem cells to create mouse embryos with beating hearts and the beginnings of muscles and blood vessels — an achievement that may bring transplantable, lab-grown organs one step closer to reality.
The challenge: By placing stem cells in the right environment, scientists can get them to develop into specific types of cells, such as the ones found in the heart or brain.
Those organoids can be used for research, but they could never be transplanted into a person.
That’s because organs have many types of cells — the heart, for example, has muscle cells, blood vessel cells, and more — and the tiny organoids we’re growing are far too simple.
The mouse embryos show more tissue types and more complexity than any previous lab creation.
Why it matters: If we could coax stem cells into developing into fully grown organs, we might be able to start growing fully transplantable body parts for people in the lab.
That would help overcome organ shortages and lead to less transplant rejection, since the replacement organs could be grown from the patient’s own stem cells.
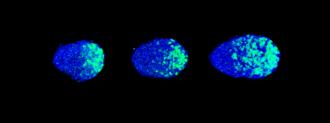
The mouse embryos: Now, scientists at the University of Virginia School of Medicine have demonstrated a technique to get stem cells to develop into mouse embryos with beating hearts — showing more tissue types and more complexity than any previous lab creation.
The embryos developed in the lab like others would grow in the womb; after about a week, they had beating hearts and were developing nerves, muscles, and other body parts.
“This is essential to be able one day to produce functional human replacement organs in a dish.”
Christine Thisse
The cold water: The embryos stopped developing about halfway through the gestation process and didn’t have everything needed to become a mouse — bits of the brain and other essential parts were missing.
However, researcher Bernard Thisse believes the team’s technique could be modified to coax the stem cells into developing into mouse embryos that would feature all of the rodent’s tissues and organs.
Looking ahead: These mouse embryos could not only lead to the development of better organoids for research, but also put us one step closer to ending organ shortages.
“This in vitro mouse model shows that we are able to induce cells to execute complex developmental programs in the right succession of steps,” research co-leader Christine Thisse said in a press release.
“This is essential to be able one day to produce functional human replacement organs in a dish,” she added.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].