This article is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.
Countless medical issues could be solved if there were simply an Amazon.com for new body parts. Heart failure? Order a new organ in your size for a transplant. Got into a car accident and broke your leg? Great news — free shipping on tibias.
Unfortunately, warehouses filled with replacement human bones, organs, and tissues don’t exist — but 3D bioprinting could lead to something even better.
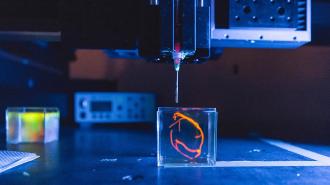
Like traditional 3D printers, these machines use computer files to create 3D objects with potentially complex structures, but instead of extruding plastic or metal, they work with bioinks containing living cells.
Because tweaking a design is as simple as making a change to a file, we could eventually see 3D bioprinters used to create personalized replacement organs, tissues, and bones, on demand — with our own cells used in the inks to prevent our bodies from rejecting the new parts.
This isn’t some far off future, either. 3D bioprinting is already creating miniature organs, patches for heart defects, and more. Here are a few of the latest examples of how the technology is being used to revolutionize healthcare, from our heads to our hearts.
Brain injury repair
Damage to the brain, whether from a stroke, a fall, or a disease, can be life threatening, and even if a person survives, the injury can leave them without the ability to think, move, and communicate the way they could before.
Trials have shown that implanting stem cells at the site of brain damage can improve some patients’ motor function, but no one has been able to get stem cells to fully reverse damage, returning the brain to its original state.
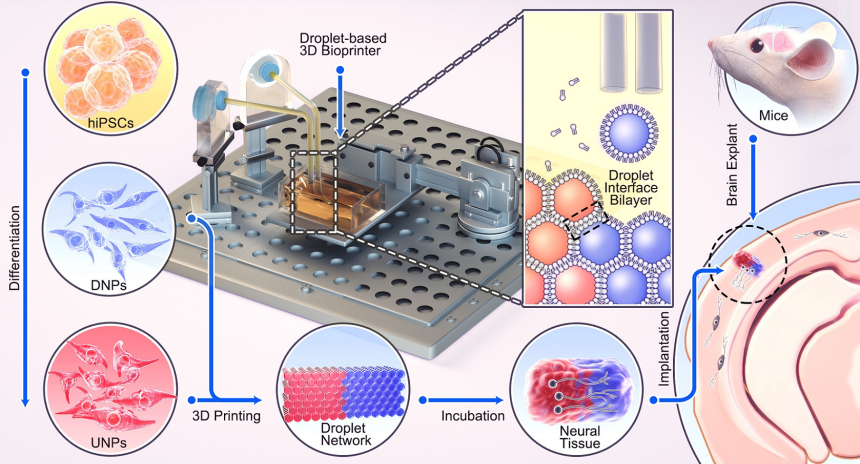
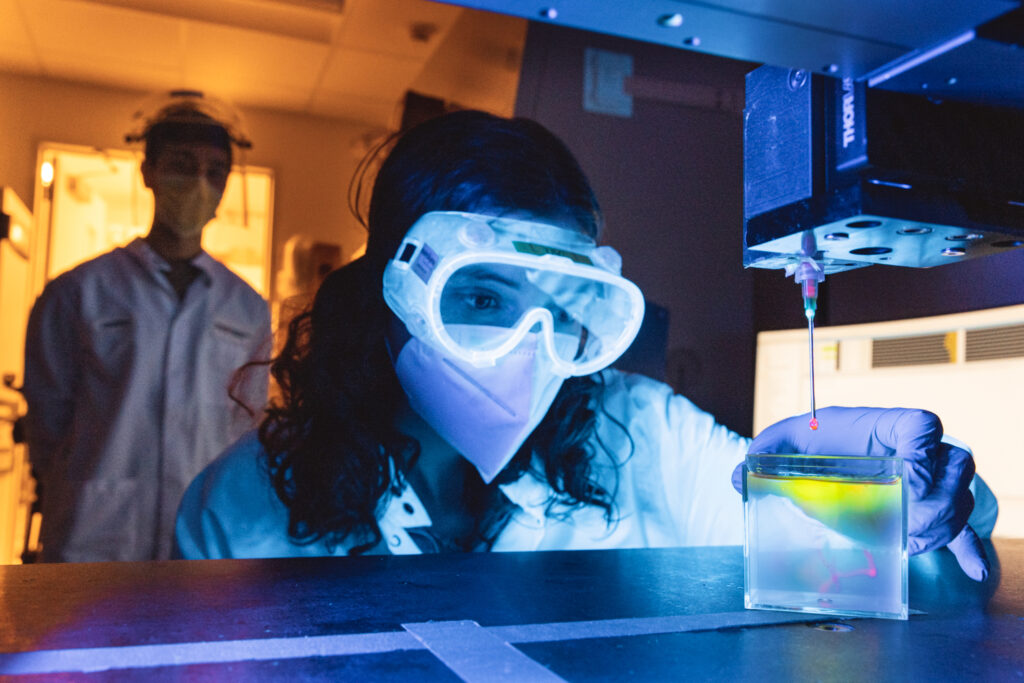
Oxford University researchers believe getting stem cells to better mimic the natural architecture of the brain will bring us closer to that goal— and that 3D bioprinting can do it.
The 3D-bioprinted stem cells successfully integrated into the mouse tissue, both structurally and functionally.
In a new study, published in Nature Communications on October 4, they created something that mimics the complex architecture of the human cerebral cortex, which has six layers — two “deep” layers and four “upper” layers — each with its own type of neuron.
They first took human induced pluripotent stem cells (HiPSCs) — adult cells that are reprogrammed back into stem cells — and coaxed them into developing into two special types of neural stem cells. One was a precursor to upper layer neurons and the other to the deep layer neurons.
Next, they created two bioinks from the neurons and printed them into a two-layer structure. When they implanted this printed tissue into slices of mouse brains, it successfully integrated into the mouse tissue, both structurally and functionally.
Researchers have yet to figure out the precise recipe to coax stem cells into developing into precursors of all six distinct types of neurons in the cerebral cortex, but the Oxford team believes its 3D bioprinting technique will be able to generate six-layered cortex tissues once that hurdle is overcome.
“[O]ur 3D printing project demonstrates substantial progress in controlling the fates and arrangements of human iPSCs to form the basic functional units of the cerebral cortex,” said senior author Zoltán Molnár.
Organs on demand
More than 6,000 people die in the US every year because they needed an organ transplant and a donor organ wasn’t available in time, but researchers at Stanford are hopeful that 3D bioprinting will be able to close that gap between supply and demand.
On September 28, they were awarded a $26.3 million contract by the National Institutes of Health’s Advanced Research Projects Agency for Health (ARPA-H) to bioprint a human heart and transplant it into a pig within the next five years.
“It’s truly a moonshot effort, but the raw ingredients for bioprinting a complete and complex human organ are now in place for this big push,” said Mark Skylar-Scott, the project’s principal investigator.
“Your own heart, made out of your own cells; that is the dream.”
Mark Skylar-Scott
Like the brain, the heart contains a great variety of cell types that have to be arranged in a precise design to work, so the Stanford team’s plan is to use stem cells to produce tons of these different types of cells in containers called “bioreactors,” which provide the ideal environment for living cells to thrive.
Using those cells as their bioink, the team will then 3D print their replica of the human heart — Skylar-Scott expects that the bioreactors will produce enough of the cells to print one heart every two weeks.
“We will use these vast numbers of cells to practice, practice, practice and learn all the design rules of the heart and optimize viability and function at the whole-heart scale for eventual implantation into a pig,” he said.
The ultimate goal is to use a person’s own stem cells as the basis for the bioink used to print their replacement heart. This would potentially eliminate the need for immunosuppression to prevent organ rejection, which leaves patients at higher risk of infection.
“Your own heart, made out of your own cells; that is the dream,” said Skylar-Scott.
Bioprinted skin
If your skin is severely damaged by a burn, disease, or injury, your doctor might perform a skin graft, where healthy skin from a different part of the body is removed and placed over the injured area.
Skin consists of three layers, and during a graft, doctors only remove the top one-and-a-half to two layers, depending on the severity of the injury. The bottommost third layer — the hypodermis — is never transplanted.
Not only do these procedures require patients to damage a part of their body that was healthy, the transplanted skin usually has a scarred appearance.
“These results show that the creation of full thickness human bioengineered skin is possible.”
Anthony Atala
On October 4, researchers from Wake Forest University published a study detailing how they used 3D bioprinting to create full-thickness skin with all three layers — something no one had done before.
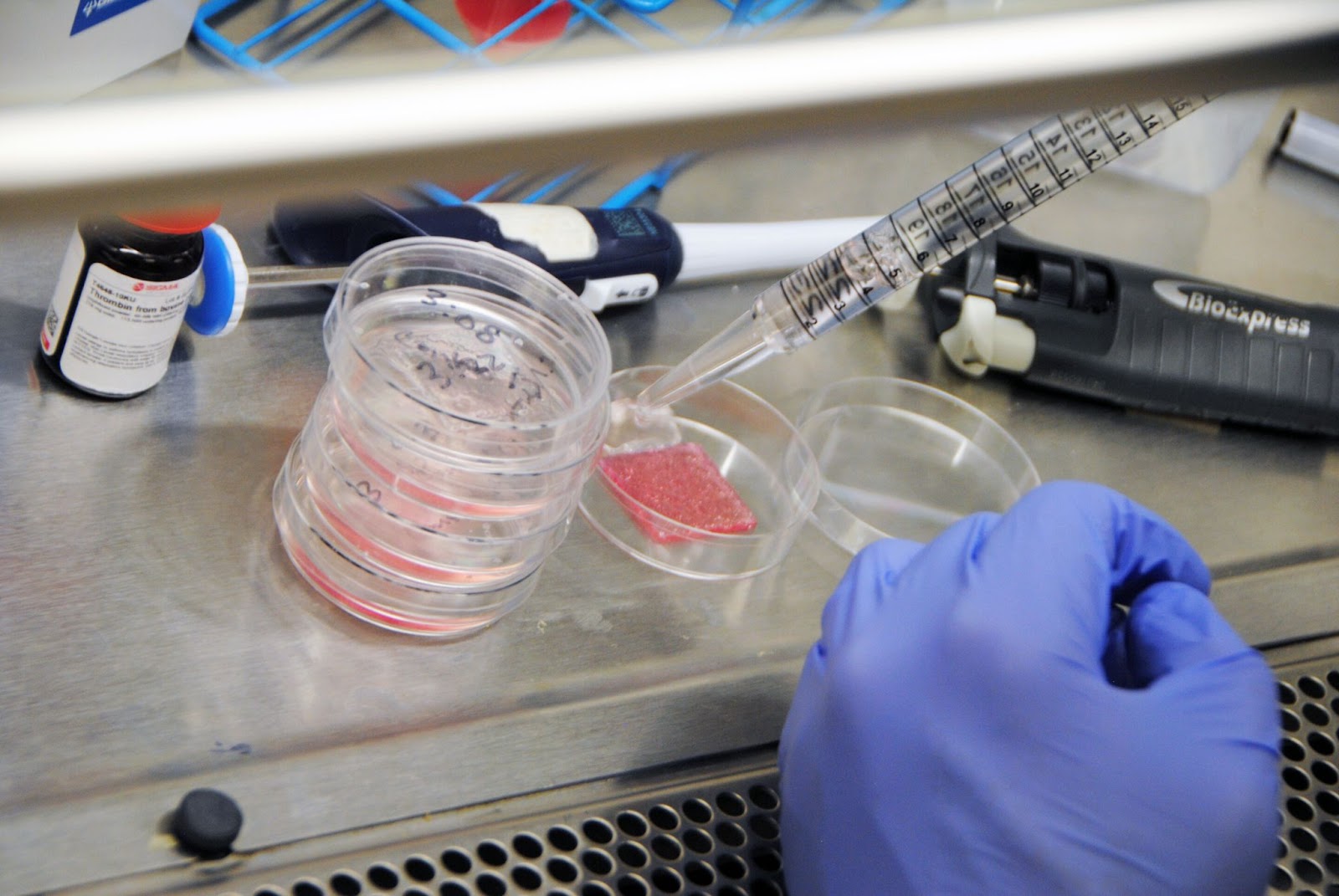
The bioinks used for the study contained a mix of hydrogels and all six of the primary cell types found in human skin, which the researchers grew in bioreactors. Using those inks, they printed the three-layered structure of real skin in petri dishes.
When the bioprinted skin was transplanted on top of wounds in mice and pigs, the injuries healed faster and showed less signs of scarring than wounds that weren’t treated.
Future studies will be needed to see how the bioprinted skin compares to traditional skin grafts, but even if it’s only as good as those, it could still free people from having to injure a healthy part of their body in order to obtain the skin needed to repair damage.
“Comprehensive skin healing is a significant clinical challenge, affecting millions of individuals worldwide, with limited options,” said primary author Anthony Atala. “These results show that the creation of full thickness human bioengineered skin is possible, and promotes quicker healing and more naturally appearing outcomes.”
Looking ahead
These are just three major advances in 3D bioprinting — ranging from the body’s largest organ (the skin) to its most vital (the brain and heart) — and the fact that they all happened in just the past few weeks should tell you how quickly the field is advancing.
In addition to these projects, other researchers are using 3D bioprinting to create new bone, cartilage, and blood vessels. Still others are developing 3D bioprinters that could print directly inside a person’s body to minimize the risks of implantation surgery.
While most of this research is still in the preclinical stage of development, some bioprinting-based treatments are already being trialed in people, and if this progress continues, it might not be long before doctors can 3D print whatever new body parts we might need.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].