This article is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.
Artificial intelligence could be the next world-changing medical breakthrough.
From autonomous surgical robots to software that spots signs of disease doctors might miss, advanced AIs are proving they could have a powerful impact on healthcare — but will patients accept Dr. AI?
Diagnostics
Doctors need to know what ails a patient in order to treat them, making diagnostics one of — if not the — most important parts of healthcare. It also might be the part where AI could have the biggest impact.
By training AIs on troves of existing data, such as patient records and medical scans, researchers have created systems capable of analyzing new cases and predicting what’s wrong — often more quickly and with similar or greater accuracy than human experts.
One of the latest examples is an AI trained to identify small bone fractures, indicating that a patient has osteoporosis, a disease that causes weak or brittle bones. If detected early, patients can take steps to strengthen their bones, but the disease often isn’t diagnosed until after a painful, potentially disabling break.
“Our AI automatically inspects the spine.”
Eren Yilmaz
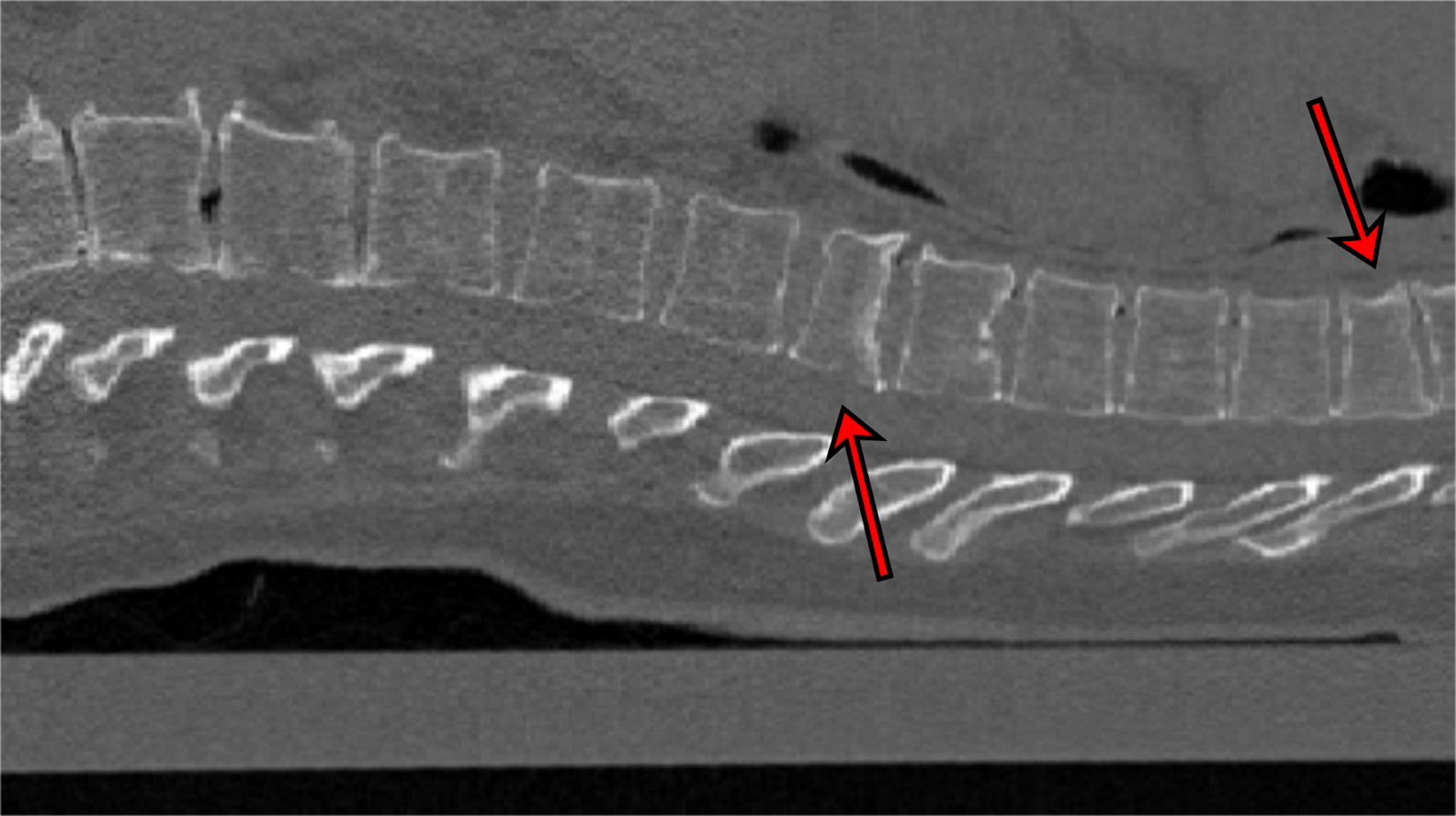
This new AI, developed by researchers in Germany, looks for the small fractures indicating osteoporosis in computed tomography (CT) scans ordered for other reasons, such as to check a patient’s lungs, and grades their severity.
“Our program can run in the background during examinations like these,” said lead author Eren Yilmaz. “It automatically inspects the spine and gives an indication of any fractures of the vertebrae that might otherwise not have been detected.”
The team tested the AI on 159 CT scans of the spine, featuring a total of 170 fractures, and it correctly classified 90% of the scans with fractures and 87% of those without. The AI is still in development, but if it makes its way into routine radiology, Yilmaz says it could be “an early warning system to prevent serious consequences of osteoporosis.”
Drug Discovery
Drug discovery typically starts with identifying a target, usually a protein, that plays a role in whatever you want to treat. If the target is “druggable” — i.e., it has a structure that allows another molecule to bind to it — the next step is finding a drug that acts on the target in a favorable way (and doesn’t cause any major problems elsewhere).
The protein cyclooxygenase, for example, is a good target for pain-relieving drugs because it creates chemicals that trigger the feeling of pain. Aspirin binds to cyclooxygenase in a way that prevents the production of those chemicals, thereby delivering pain relief.
We have an estimated 3,000 druggable proteins in our bodies and a near infinite number of potential drugs that could affect them, so finding a pairing that does what we want safely is a slow, expensive process — the kind that AI is now disrupting.
“We are proud to be … one of the few AI-driven biotech companies to have made it to the clinical stage.”
Alice Zhang
In October 2022, biotech company Verge Genomics began the one of first clinical trials of an AI-discovered drug candidate, which aims to treat ALS, also known as Lou Gehrig’s Disease.
Verge identified this drug, a molecule called VRG50635, after feeding an AI more than 11 million data points from genetics databases and ALS patient tissue samples. The system then identified a protein called PIKfyve as potentially playing a role in the disease and suggested that VRG50635 should be able to inhibit it.
“We are proud to be not just one of the few AI-driven biotech companies to have made it to the clinical stage, but also one of the first to bring forward a novel clinical compound against a novel target, that was entirely discovered and developed internally on our platform,” said Verge CEO Alice Zhang.
“This is a significant milestone for both longevity research and the application of AI to drug discovery.”
Felix Wong
Even more recently, biotech company Integrated Biosciences announced that it had trained an AI to find drugs likely to clear out senescent cells — “zombie” cells that have stopped multiplying but also haven’t died — which are linked to many age-related diseases.
Some scientists suspect that drugs that can get rid of them, called “senolytics,” could help us live longer, healthier lives. The field is still relatively new, though, and only a few candidates have made it to clinical trials.
From a collection of more than 800,000 molecules, Integrated’s AI was able to identify three new senolytics with desirable properties (such as signs of high oral bioavailability, meaning you can potentially take it as a pill). One of the drugs was shown to clear senescent cells as hoped in experiments on aged mice.
“This research result is a significant milestone for both longevity research and the application of artificial intelligence to drug discovery,” said Felix Wong, co-founder of Integrated Biosciences.
“These data demonstrate that we can explore chemical space in silico and emerge with multiple candidate anti-aging compounds that are more likely to succeed in the clinic, compared to even the most promising examples of their kind being studied today,” he continued.
Robotics
Today, instead of just hunching over bodies and wielding scalpels, many surgeons stand behind computer monitors, using joysticks to precisely guide the robotic arms they see on screen through a patient’s body.
These robots can make it easier for doctors to do complex, delicate surgeries, while minimizing risk and pain, but they still depend on the know-how and skill of the doctor behind the joystick — for now.
The AI robot did the job more precisely and quickly than a human surgeon.
In January 2022, Johns Hopkins University (JHU) reported that its AI-powered Smart Tissue Autonomous Robot (STAR) had performed a delicate surgery on live pigs, suturing together two ends of intestine.
Not only was this the first example of a robot performing an autonomous laparoscopic surgery, but the bot also did the job more precisely and more quickly than a human surgeon.
“By incorporating novel suturing tools, imaging systems, machine learning algorithms, and robotic controls, the STAR system is equipped to overcome the challenges of autonomous laparoscopic surgery in soft tissues,” said senior author Axel Krieger.

The big picture
The JHU team says STAR could make surgery more predictable, affordable, and available — patient outcomes would no longer be tied to the skill of the surgeons at their local hospital — but notes that their robot faces the same hurdle as other AIs in healthcare: a public wary of letting AI contribute to their medical care.
In February 2023, Pew Research Center reported the results of a survey gauging Americans’ acceptance of AI in medicine, and 60% of respondents said they’d feel uncomfortable if their doctor relied on AI to diagnose their disease or decide on treatments. Only 38% believed it would lead to better health outcomes.
“In many ways, our work highlights a potential blind spot among AI researchers.”
Sanjay Aneja
Meanwhile, more than 70% of respondents to a similar survey, conducted by Yale Cancer Center in 2022, said they would be at least somewhat uncomfortable receiving a diagnosis from an AI that can’t explain how it reached a certain conclusion — even if it was 90% accurate.
The Yale survey also found that patient comfort varied depending on what the AI was doing — 55% of respondents said they’d be at least somewhat comfortable having an AI read chest radiographs, but that number dropped to 31.2% if the AI was diagnosing cancer.
To maximize the potential benefits of AI in medicine, developers need to focus not only on training the AIs, but also thinking about what patients hope to gain from them and how best to alleviate their concerns.
“In many ways, our work highlights a potential blind spot among AI researchers, which needs to be addressed as these technologies become more common in clinical practice,” said Sanjay Aneja, senior author of the Yale study.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].





